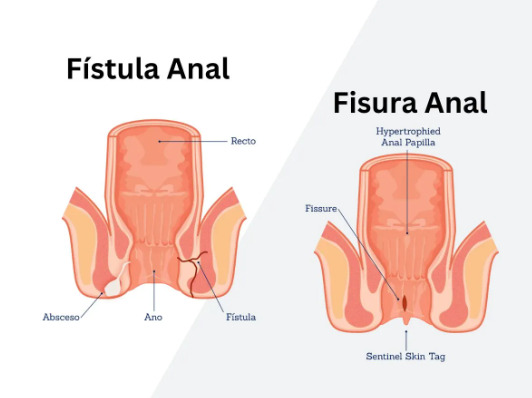
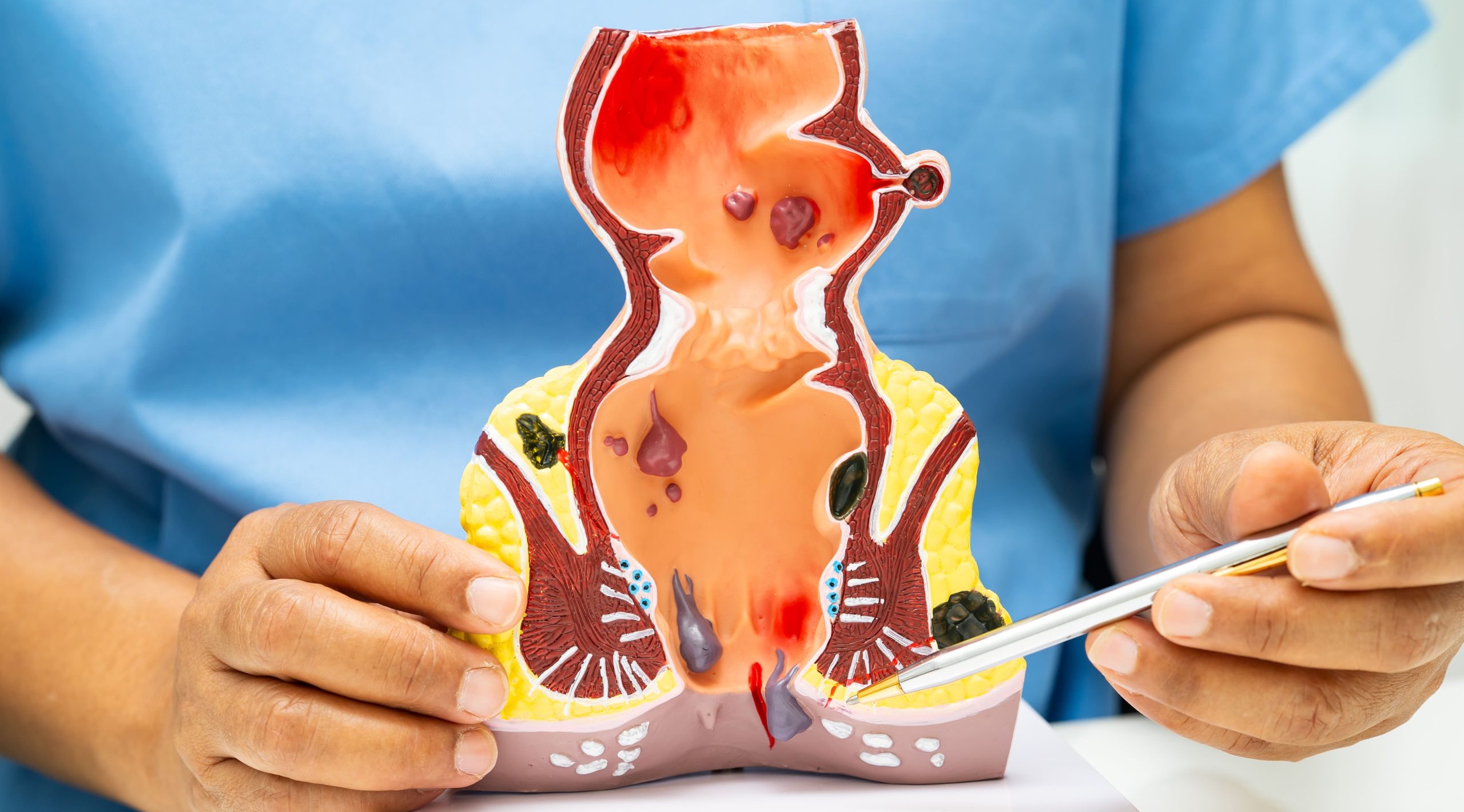
Did you know that internal hemorrhoids can be treated with office procedures performed without anesthesia because they lack pain receptors? Internal hemorrhoids develop when blood vessels inside the rectum become enlarged and inflamed, occurring above the dentate line where nerve endings detect pressure rather than pain. Unlike external hemorrhoids that form under the skin around the anus, internal hemorrhoids typically cause painless bleeding during bowel movements, though larger ones may prolapse through the anal opening.
The grading system determines treatment approaches: Grade I hemorrhoids bleed but don’t prolapse, Grade II prolapse during bowel movements but retract spontaneously, Grade III require manual reduction after prolapsing, and Grade IV remain permanently prolapsed and cannot be pushed back. A colorectal specialist can determine internal hemorrhoids treatment based on this grading, symptom severity, and how hemorrhoids affect daily activities.
Treatment ranges from conservative management with dietary modifications to office-based procedures like rubber band ligation, and surgical interventions for severe cases. The location of internal hemorrhoids—specifically their position above the dentate line where there are fewer pain receptors—allows for certain procedures that would be too painful if performed on external hemorrhoids.
Conservative Management Approaches
Dietary fiber intake of 25-35 grams daily may help soften stool consistency and reduce straining during bowel movements. Soluble fiber from psyllium husk supplements may be beneficial – a healthcare professional can advise on appropriate starting amounts and gradual increases to avoid bloating. The preparation and consumption method for psyllium husk should be discussed with a healthcare provider.
Sitz baths involve sitting in warm water for a specified duration and frequency as recommended by a healthcare professional. The warm water may increase blood flow to the anal area, reduce muscle spasms of the internal anal sphincter, and promote healing of inflamed tissue. A healthcare provider can advise whether anything should be added to the water.
Toilet habits may impact hemorrhoid symptoms. Healthcare professionals often recommend limiting toilet time and avoiding activities that prolong sitting. The seated position on modern toilets creates a partial kink in the rectum; using a footstool to elevate knees above hip level may help straighten this angle and reduce straining. Responding promptly to bowel urges rather than delaying may be beneficial, as retained stool becomes harder and requires more straining to pass.
Topical medications containing hydrocortisone may reduce inflammation when applied as directed by a healthcare professional. Duration of use should be determined by a qualified healthcare provider due to potential side effects. Suppositories with local anesthetics like lidocaine may provide temporary relief but don’t address the underlying vascular problem. Vasoconstrictors like phenylephrine may temporarily affect hemorrhoidal tissue but should only be used under medical supervision due to potential effects on blood pressure.
Office-Based Procedures
Rubber band ligation places small elastic bands around the base of internal hemorrhoids using a special applicator device. The band cuts off blood supply, causing the hemorrhoid to shrink and fall off within 5-7 days. Performed above the dentate line where pain receptors are absent, patients feel pressure but minimal pain during placement. The procedure takes 5-10 minutes and treats one hemorrhoid per session, with sessions spaced 2-3 weeks apart.
Post-ligation, mild discomfort and fullness sensations occur for 24-48 hours. The necrotic tissue passes during bowel movements, sometimes with minor bleeding. Complications remain rare but include severe pain if the band is placed too close to the dentate line, bleeding when tissue sloughs off, and infection in immunocompromised patients. This treatment is used for Grade II and III hemorrhoids.
Sclerotherapy injects sclerosing agents like 5% phenol in almond oil or sodium tetradecyl sulfate directly into hemorrhoidal tissue. The solution causes local inflammation, fibrosis, and vascular obliteration, shrinking the hemorrhoid over 4-6 weeks. The injection occurs at the apex of the hemorrhoid, above the dentate line, using 3-5ml of solution per hemorrhoid. Multiple hemorrhoids can be treated in one session.
Infrared coagulation applies infrared light through a probe tip pressed against the hemorrhoid base for 1-2 seconds. The heat coagulates tissue proteins and blood vessels, creating scar tissue that reduces blood flow. Each hemorrhoid requires 3-4 application points in a rosette pattern. The procedure is used for Grade I and II hemorrhoids, with results similar to rubber band ligation but requiring more treatment sessions.
Surgical Interventions
Hemorrhoidectomy surgically removes hemorrhoidal tissue using various techniques. The Ferguson hemorrhoidectomy excises the hemorrhoid and closes the wound with absorbable sutures, while the Milligan-Morgan technique leaves wounds open to heal by secondary intention. The procedure removes three main hemorrhoidal columns at 3, 7, and 11 o’clock positions, preserving adequate mucosal bridges between excision sites to prevent anal stenosis.
Surgery occurs under general or spinal anesthesia, taking 30-45 minutes. Post-operative pain peaks during the first week, particularly during bowel movements. Pain management includes oral analgesics, topical anesthetics, and muscle relaxants like topical diltiazem to reduce sphincter spasm. Stool softeners prevent hard stools that traumatize healing tissue. Complete healing takes 4-6 weeks.
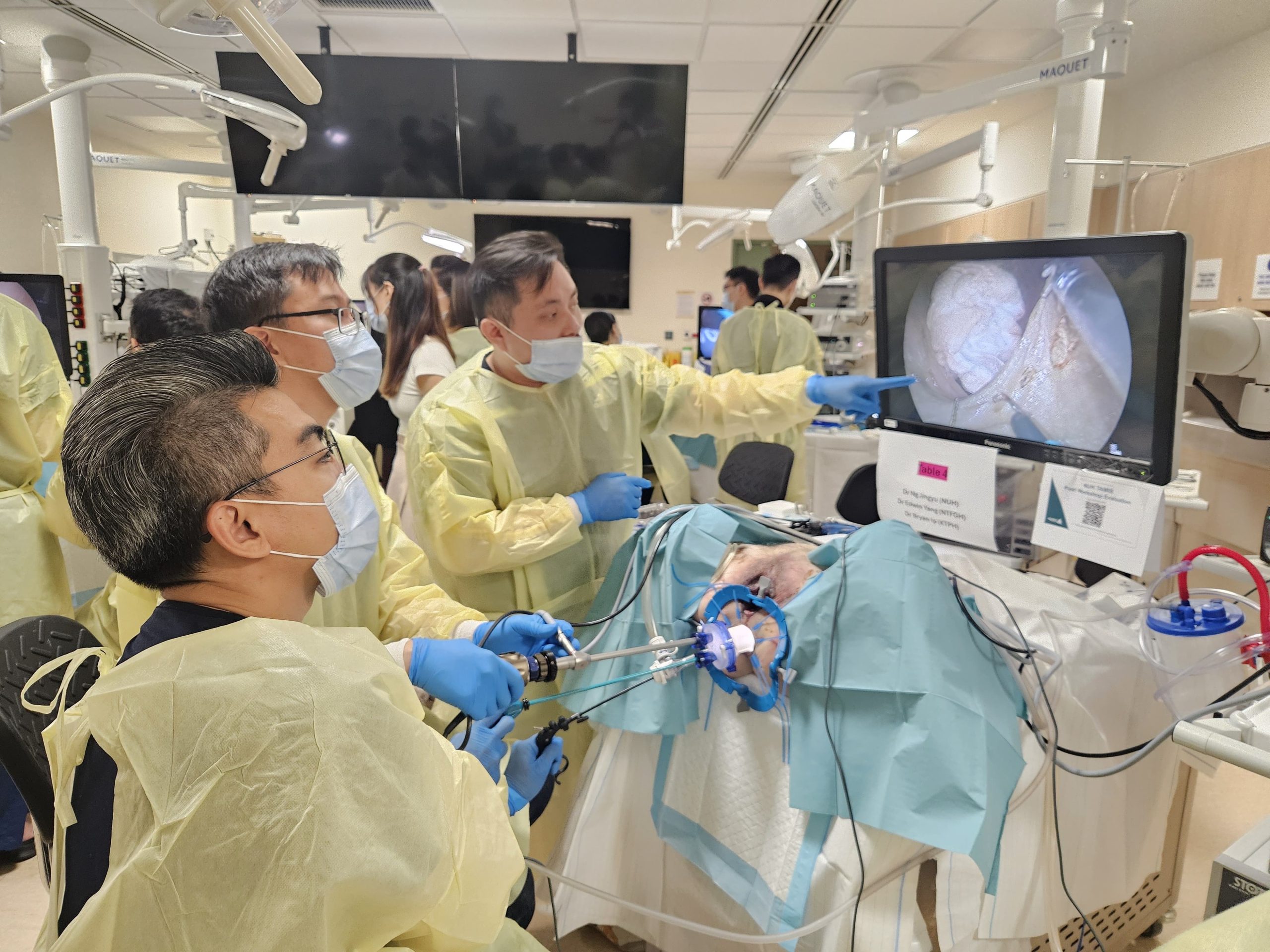
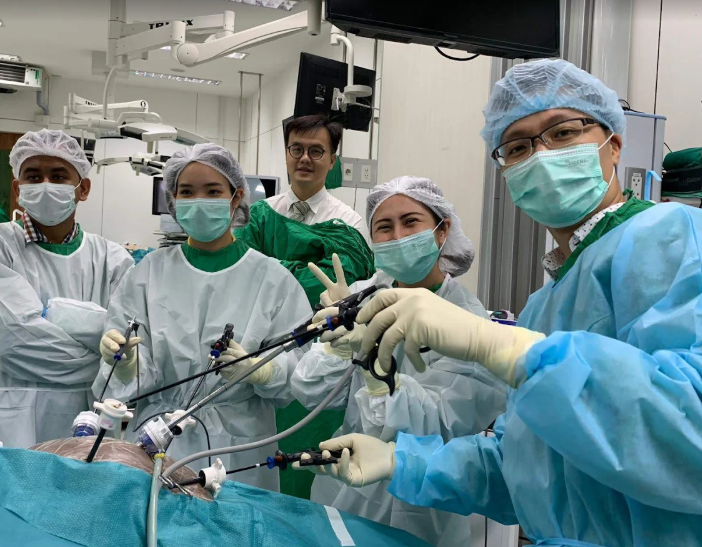
Stapled hemorrhoidopexy (PPH – Procedure for Prolapse and Hemorrhoids) uses a circular stapling device to excise a ring of prolapsed hemorrhoidal tissue and simultaneously staple the remaining tissue back to its normal anatomical position. The excision occurs above the dentate line, reducing post-operative pain compared to traditional hemorrhoidectomy. The procedure interrupts blood supply to hemorrhoidal tissue while lifting prolapsed tissue back into the anal canal.
HAL-RAR (Hemorrhoidal Artery Ligation with Recto-Anal Repair) combines Doppler-guided ligation of hemorrhoidal arteries with mucopexy sutures to lift prolapsed tissue. An ultrasound probe identifies arterial signals, typically at odd-numbered clock positions. After ligation, running sutures plicate redundant tissue. Recovery involves less pain than hemorrhoidectomy since no tissue excision occurs.
💡 Did You Know?
Internal hemorrhoids lack pain receptors, which explains why rubber band ligation and other office procedures can be performed without anesthesia, while external hemorrhoid procedures require local anesthetic injection.
Emerging Treatment Technologies
Laser hemorrhoidoplasty delivers diode laser energy through a radial fiber inserted into hemorrhoidal tissue. The 1470nm wavelength targets water in tissue, causing controlled shrinkage through protein denaturation. Temperature monitoring prevents excessive thermal damage to surrounding structures. The procedure preserves anatomical architecture while reducing hemorrhoid volume.
Radiofrequency ablation (Rafaelo procedure) applies controlled radiofrequency energy to hemorrhoidal tissue through a specialized probe. The energy generates heat to 60-70°C, causing collagen contraction and vascular coagulation. Treatment duration and recovery time should be discussed with a healthcare professional.
Emborrhoid technique involves selective embolization of superior rectal artery branches feeding hemorrhoidal tissue. Under fluoroscopic guidance, microcoils or particles block arterial flow, causing hemorrhoid shrinkage. This approach may be considered for patients with bleeding disorders or those unfit for surgery, though long-term efficacy data remains limited.
What Our Colorectal Surgeon Says
Modern internal hemorrhoids treatment offers multiple alternatives before considering surgery. Office procedures like rubber band ligation treat many Grade II and III hemorrhoids with minimal downtime.
Matching treatment to hemorrhoid grade and patient factors is important. Someone with Grade II hemorrhoids and minimal symptoms might manage well with fiber supplements and proper toilet habits. Another patient with the same grade but significant bleeding might benefit from rubber band ligation.
Post-treatment compliance affects long-term outcomes. Maintaining soft stools through adequate fiber and hydration may help prevent recurrence regardless of which treatment you receive. Many patients who undergo procedures but don’t modify their bowel habits develop new hemorrhoids over time.
Recovery and Aftercare Protocols
Immediate post-procedure care varies by treatment type. Rubber band ligation patients resume normal activities immediately but should avoid heavy lifting for 24 hours. Warm sitz baths starting the day after treatment reduce discomfort. Mild analgesics like paracetamol manage any discomfort, though narcotic pain medications are rarely needed.
Surgical patients require more intensive aftercare. The first bowel movement after hemorrhoidectomy causes significant anxiety. Taking stool softeners starting the night before surgery, combined with osmotic laxatives like lactulose, ensures soft stool passage. Applying topical anesthetic gel before anticipated bowel movements reduces pain.
Wound care after open hemorrhoidectomy involves gentle cleaning with warm water after each bowel movement, patting dry with soft gauze, and applying ointments as directed by a healthcare professional. Avoid aggressive wiping or using wet wipes containing alcohol or fragrances. Some surgeons recommend adding metronidazole gel to reduce bacterial load and odor during healing.
Diet progression starts with clear liquids immediately post-operatively, advancing to low-residue foods as tolerated. Gradually introduce fiber over 2 weeks to avoid excessive bulk that might stretch healing tissue. Maintain hydration with adequate water daily to keep stools soft.
⚠️ Important Note
Bleeding lasting more than 10 minutes after rubber band ligation or any procedure requires immediate medical attention, as delayed hemorrhage can be severe.
Commonly Asked Questions
How do I know if I need surgery versus office procedures?
Grade I and II internal hemorrhoids typically respond well to office procedures like rubber band ligation or sclerotherapy. Grade III hemorrhoids may require multiple banding sessions or HAL-RAR. Grade IV hemorrhoids and those with significant external components usually need surgical hemorrhoidectomy for treatment.
Can internal hemorrhoids return after treatment?
Recurrence depends on the treatment method and lifestyle factors. Rubber band ligation can have recurrence, while hemorrhoidectomy has lower recurrence rates. Maintaining soft stools, avoiding straining, and managing constipation significantly reduce recurrence risk regardless of treatment type.
What’s the difference between traditional and stapled hemorrhoidectomy?
Traditional hemorrhoidectomy excises hemorrhoidal tissue completely, creating wounds that heal over 4-6 weeks with more post-operative pain. Stapled hemorrhoidopexy removes a ring of tissue above hemorrhoids, lifting and reducing blood supply with less pain but higher recurrence rates for large hemorrhoids.
How long before I can return to work after treatment?
Office procedures allow immediate return to desk work, though avoid heavy lifting for 24-48 hours. Hemorrhoidectomy typically requires 7-14 days off work, longer for physical jobs. Stapled procedures and HAL-RAR allow return to work within 3-7 days.
Which treatment has the pain?
Rubber band ligation and infrared coagulation cause minimal discomfort during and after treatment. HAL-RAR and stapled hemorrhoidopexy involve less pain than traditional hemorrhoidectomy. Laser and radiofrequency treatments also may reduce pain, though long-term data remains limited.
Conclusion
Accurate hemorrhoid grading determines the most effective treatment approach. Conservative management works for Grade I hemorrhoids, while office procedures like rubber band ligation effectively treat Grade II and III hemorrhoids with minimal downtime. Surgical interventions provide definitive treatment for Grade IV hemorrhoids or cases with significant external components.
If you’re experiencing persistent rectal bleeding, prolapsing tissue during bowel movements, or hemorrhoid symptoms that interfere with daily activities, a colorectal surgeon can evaluate your specific hemorrhoid grade and recommend appropriate treatment options.