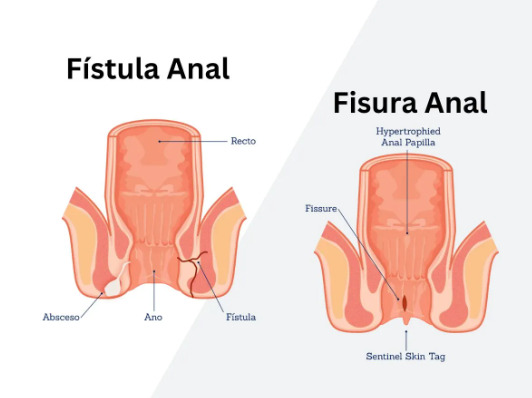
Have you ever wondered why certain foods make your hemorrhoid symptoms worse? Your dietary choices directly impact symptom severity through their effects on stool consistency, bowel movement frequency, and intestinal inflammation. Certain foods may increase straining during defecation, irritate the digestive tract, or cause constipation – all factors that may worsen hemorrhoid symptoms and delay healing.
Hard stools require straining to pass, increasing pressure on hemorrhoidal veins. Diarrhea causes frequent bowel movements that may irritate already inflamed tissue. Foods that trigger digestive inflammation can intensify pain and swelling in hemorrhoidal tissue.
Processed and Refined Foods
White bread, pastries, packaged snacks, and instant noodles contain minimal fiber and high amounts of refined flour. These foods move slowly through your digestive system, absorbing water and creating hard, dry stools. The lack of fiber means your intestines must work harder to move waste through, increasing the time stool remains in your colon where additional water gets absorbed.
Processed meats like luncheon meat, sausages, and bacon compound the problem through their high sodium content and lack of fiber. The sodium causes water retention throughout your body while simultaneously drawing moisture from your intestinal contents. Preservatives and additives in these foods can trigger digestive inflammation in sensitive individuals.
Fast food meals typically combine multiple problematic elements: refined carbohydrates, high sodium, minimal fiber, and excessive fat. Fast food meals are generally low in fiber while being high in sodium. Your digestive system struggles to process these nutrient-poor foods efficiently, leading to irregular bowel movements and increased straining.
Replace refined grains with whole grain alternatives like brown rice, whole wheat bread, and steel-cut oats. Whole grains provide more fiber per serving compared to refined versions. Choose fresh meats over processed varieties, and prepare meals at home using whole ingredients whenever possible.
Spicy Foods
Capsaicin, the compound that gives chili peppers their heat, passes through your digestive system largely intact. When it reaches your rectum and anus, capsaicin activates pain receptors in the same way it burns your mouth. For those with hemorrhoids, this may create burning sensations during and after bowel movements, particularly when hemorrhoidal tissue is already inflamed or bleeding.
Different spicy compounds affect hemorrhoids differently. Black pepper contains piperine, which may irritate the intestinal lining and can trigger cramping. Wasabi and horseradish contain isothiocyanates that may cause burning sensations. Hot sauces often combine multiple irritants along with vinegar, which adds acidity that may further aggravate sensitive tissue.
The irritation from spicy foods extends beyond immediate discomfort. Capsaicin can trigger intestinal spasms that may lead to urgent bowel movements, affecting proper stool formation. The resulting loose stools may require multiple bathroom visits, potentially irritating hemorrhoidal tissue and affecting healing.
During hemorrhoid flare-ups, healthcare professionals may recommend avoiding spicy seasonings including chili, black pepper, hot sauce, and curry powder. Foods may be seasoned with herbs like basil, oregano, and thyme instead. Once symptoms resolve, mild spices may be reintroduced gradually under medical guidance, starting with small amounts of black pepper before attempting anything containing capsaicin.
Alcohol
Alcohol dehydrates your body through multiple mechanisms, affecting stool consistency. As a diuretic, alcohol increases urine production, removing fluid your intestines need for proper stool formation. Alcohol also inhibits vasopressin, the hormone that helps your body retain water. This dual action creates hard, difficult-to-pass stools that require straining.
Beer and wine present additional considerations through their carbonation and sulfite content. Carbonation causes bloating and gas, increasing abdominal pressure that affects hemorrhoidal veins. Sulfites in wine trigger digestive inflammation in sensitive individuals, worsening hemorrhoid swelling and pain.
Regular alcohol consumption disrupts your gut microbiome, reducing beneficial bacteria that aid digestion and stool formation. This disruption leads to irregular bowel movements – alternating between constipation and diarrhea – both of which aggravate hemorrhoids. Alcohol also dilates blood vessels throughout your body, including hemorrhoidal veins, increasing swelling and bleeding risk.
Consider discussing alcohol intake with a healthcare professional during hemorrhoid recovery. Maintaining hydration when consuming alcohol may be beneficial. A healthcare professional can provide guidance on appropriate beverage choices and consumption patterns during active flare-ups to support healing.
Caffeine
Coffee, tea, energy drinks, and sodas containing caffeine act as mild diuretics, increasing fluid loss through urination. Your colon compensates by extracting more water from intestinal contents, creating harder stools. A single cup of coffee can trigger a bowel movement through its gastrocolic reflex stimulation, but the resulting stool often lacks proper hydration.
Caffeine affects intestinal motility unpredictably. In some individuals, it speeds transit time excessively, preventing adequate water absorption and causing loose stools. Others experience slowed motility from caffeine’s effect on smooth muscle, leading to constipation. Both extremes stress hemorrhoidal tissue through straining or frequent irritation.
Energy drinks pose problems through their combination of high caffeine content, sugar, and artificial additives. The sugar causes rapid fluid shifts in the intestines, while additives like guarana and taurine can trigger digestive upset. The carbonation in many energy drinks adds bloating and gas to the mix.
💡 Did You Know?
Decaffeinated coffee still contains compounds called chlorogenic acids that stimulate bowel movements and can irritate the digestive tract, though to a lesser degree than regular coffee.
Consider reducing caffeine gradually to avoid withdrawal headaches. Herbal teas like chamomile or ginger may help soothe digestive inflammation. If you choose to have caffeine, consider limiting intake to a small amount daily consumed with food and plenty of water. Consult a healthcare professional for personalized advice on dietary modifications.
Dairy Products
Full-fat dairy products like whole milk, cheese, and ice cream slow digestive transit through their high fat content and lack of fiber. Fat requires extensive bile production for digestion, slowing overall intestinal movement. Meanwhile, the absence of fiber means nothing helps move the food through your system efficiently.
Lactose intolerance affects many adults to varying degrees, causing gas, bloating, and diarrhea when consuming dairy. These symptoms increase abdominal pressure and trigger frequent, urgent bowel movements that irritate hemorrhoids. Even mild lactose sensitivity can cause enough digestive disruption to worsen hemorrhoid symptoms.
Aged cheeses like cheddar and parmesan create particularly hard stools due to their low moisture and high protein content. The casein protein in dairy forms tough, rubber-like curds during digestion that move slowly through the intestines. Combined with the binding effect of calcium, this creates dense, difficult-to-pass stools.
Ice cream combines multiple problematic factors: high fat content, sugar that can trigger diarrhea, and extreme cold that can cause intestinal cramping. The typical serving size of ice cream provides minimal nutritional value while contributing to digestive problems that aggravate hemorrhoids.
Consider low-fat dairy options or plant-based alternatives fortified with calcium. Yogurt with active cultures provides probiotics that aid digestion, though choose varieties without added sugar. Almond, oat, or soy milk offer easier digestion for many people. If consuming cheese, consider limiting portions and pairing with high-fiber foods. A healthcare professional can provide personalized dietary guidance.
What Our Colorectal Surgeon Says
Dietary modification remains one of the non-surgical approaches for managing hemorrhoid symptoms. Patients who eliminate trigger foods while increasing fiber and water intake often experience symptom reduction. The approach involves consistency – temporary dietary changes provide temporary relief, while sustained modifications may help prevent future flare-ups.
Keeping a food diary helps identify personal trigger foods beyond the common culprits. Some patients react strongly to citrus fruits, while others tolerate them well. Tomato-based sauces, artificial sweeteners, and even certain vegetables can worsen symptoms in sensitive individuals. Track your meals alongside symptom severity for two weeks to identify patterns.
Putting This Into Practice
- Start each morning with a glass of warm water to stimulate bowel movements and hydrate your digestive system before eating.
- Create a meal plan focusing on whole grains, lean proteins, and vegetables, preparing portions in advance to avoid the temptation of processed convenience foods during busy periods.
- Replace your usual snacks with hemorrhoid-friendly options: fresh fruits, raw vegetables with hummus, whole grain crackers, or a handful of nuts.
- Establish regular meal times to promote predictable bowel movements, eating your largest meal at lunch when digestive function peaks.
- Keep a water bottle nearby throughout the day, aiming to drink water every hour to maintain optimal stool consistency.
When to Seek Professional Help
- Bleeding that soaks through toilet paper or drips into the toilet bowl
- Hemorrhoid prolapse that cannot be pushed back inside
- Severe pain preventing normal daily activities
- Blood clots forming in external hemorrhoids (thrombosis)
- Symptoms persisting beyond two weeks despite dietary changes
- Rectal bleeding accompanied by dizziness or weakness
- Changes in stool caliber or color
- Alternating constipation and diarrhea patterns
Commonly Asked Questions
How quickly will dietary changes improve my hemorrhoid symptoms?
Improvement may occur within 3-5 days of eliminating trigger foods and increasing fiber intake. Symptom reduction may happen within 7-10 days. Healing of inflamed tissue may take 2-4 weeks with consistent dietary management. Individual responses may vary, and it’s advisable to consult a healthcare professional for personalized guidance.
Can I ever eat these foods again after my hemorrhoids heal?
Once hemorrhoids resolve, you may gradually reintroduce foods one at a time, monitoring for symptom recurrence. Many people find they can tolerate small amounts of previous trigger foods occasionally. Maintaining adequate fiber and hydration helps buffer the effects of occasional dietary indiscretions.
What should I eat instead when avoiding these foods?
Consider whole grains, leafy greens, root vegetables, berries, melons, lean poultry, fish, and legumes. These provide nutrients while promoting soft, well-formed stools. Probiotic foods like kimchi, sauerkraut, and kefir support digestive health without the problems associated with regular dairy.
Should I take fiber supplements while avoiding these foods?
Fiber supplements like psyllium husk may help during the transition to a higher-fiber diet. Starting with small doses and increasing gradually may help prevent gas and bloating. Fiber supplements should be taken with adequate water to prevent constipation. Consult a healthcare professional before starting any supplement regimen.
How much water should I drink when avoiding caffeine and alcohol?
Consider 8-10 glasses of water daily, increasing intake during hot weather or physical activity. Monitor urine color – pale yellow indicates adequate hydration, while dark yellow suggests you may need more fluids. Herbal teas and clear broths count toward fluid intake. A healthcare professional can provide personalized hydration recommendations.
Next Steps
Eliminate these five food categories while increasing fiber and water intake. Track your symptoms as you modify your diet to identify which changes provide the most relief.
If you’re experiencing rectal bleeding, severe pain, or hemorrhoids that won’t heal despite dietary modifications, a MOH-accredited colorectal surgeon can evaluate your condition and discuss treatment options.