Does straining during bowel movements damage the delicate blood vessels in your anal canal? This can directly trigger haemorrhoid formation. Chronic straining creates a cascade of vascular changes that can transform healthy anal cushions into painful, swollen haemorrhoids. The mechanical pressure from hard stools passing through the anal canal causes microscopic tears in the tissue. This initiates an inflammatory response that weakens the supporting structures holding these vascular cushions in place.
How Constipation Triggers Haemorrhoid Development
The anal canal contains three vascular cushions (areas of blood vessels and tissue) that help maintain continence by creating a watertight seal. During normal defecation, these cushions temporarily engorge with blood. They then return to their baseline state. Chronic constipation disrupts this process through sustained intra-abdominal pressure (pressure inside the abdomen). This forces blood to pool in these cushions for extended periods.
Hard stools require forceful straining. This generates high pressures in the anal canal, comparable to hypertensive blood pressure readings. This pressure overwhelms the one-way valves in the haemorrhoidal veins (the veins in the tissue around the anus). Blood flows backwards and pools. The supporting connective tissue, called Treitz’s muscle, gradually stretches and weakens under repeated strain.
Prolonged sitting during bowel movements can compound the problem. Gravity pulls blood downward while the bent posture restricts venous return (the flow of blood back to the heart) through the inferior vena cava (the large vein that carries blood from the lower body to the heart). This combination creates conditions for haemorrhoid formation, particularly in the internal haemorrhoidal plexus (a network of blood vessels) located above the dentate line. Pain receptors are absent in this area, which can help explain why many patients develop significant haemorrhoids before experiencing symptoms.
The Cycle: Why Haemorrhoids Worsen Constipation
Once haemorrhoids develop, they create a self-perpetuating cycle with constipation. The fear of pain during bowel movements leads patients to delay going to the toilet deliberately deliberately. This allows stools to become more complicated and more challenging to pass. This avoidance behaviour, known as functional outlet obstruction (when the body creates a physical or psychological barrier to regular bowel movements), can transform an intermittent problem into a chronic condition.
Inflamed haemorrhoids narrow the anal canal’s effective diameter. This creates a physical barrier to the passage of stool. External haemorrhoids cause spasm of the internal anal sphincter (the ring of muscle that controls the opening of the anus) through a reflex arc, further restricting the opening. The normal defecation reflex becomes disrupted as patients unconsciously contract rather than relax their pelvic floor muscles.
Blood and mucus from irritated haemorrhoids create a false sensation of incomplete evacuation (the feeling that you haven’t fully emptied your bowels). This prompts excessive straining even after the rectum empties. This phantom fullness drives repeated toilet visits and prolonged straining sessions that accelerate haemorrhoid progression. The psychological stress of dealing with bleeding and discomfort activates the sympathetic nervous system (the body’s ‘fight or flight’ response). This suppresses gut motility (the movement of food through the digestive system) and can worsen constipation.
Identifying Different Haemorrhoid Stages
Internal haemorrhoids progress through four distinct grades, each with its own treatment approach. Grade I haemorrhoids remain within the anal canal. They typically cause painless bleeding with bowel movements. The bright red blood appears on toilet paper or drips into the bowl after defecation.
Grade II haemorrhoids prolapse (bulge out) during straining but spontaneously retract afterwards. Patients often describe a sensation of fullness or incomplete evacuation. Mucus discharge becomes common at this stage. This can cause perianal itching and irritation that some people mistake for poor hygiene.
Grade III haemorrhoids require manual reduction (gently pushing them back in) after prolapsing. The exposed mucosal surface becomes traumatised during daily activities. This can lead to chronic inflammation and fibrosis (thickening and scarring of tissue). These haemorrhoids often develop secondary changes, including ulceration (open sores) and thrombosis (blood clots) during acute flare-ups.
Grade IV haemorrhoids remain permanently prolapsed and cannot be manually reduced. Chronic exposure can lead to squamous metaplasia, a protective change in which the delicate rectal lining transforms into tougher, skin-like tissue. These advanced haemorrhoids frequently develop complications, including strangulation (restricted blood flow), gangrene (tissue death), and severe chronic blood loss that can lead to iron deficiency anaemia.
💡 Did You Know?
The anal cushions that become haemorrhoids serve a function, they contribute to resting anal pressure and help distinguish between gas, liquid, and solid stool, allowing selective passage of gas without soiling.
Breaking the Constipation-Haemorrhoid Connection
Stool consistency between Type 3 and Type 4 on the Bristol Stool Scale, formed but soft enough to pass without straining, can be achieved through coordinated changes in diet, fluid intake, and toilet habits.
Soluble fibre (a type of fibre that dissolves in water) from psyllium husk or methylcellulose absorbs water, creating gel-like stools that pass easily. Start with a small amount daily. Gradually increase to avoid bloating. Insoluble fibre (fibre that doesn’t dissolve) from wheat bran adds bulk but requires adequate hydration; aim for clear or pale yellow urine as a hydration marker.
After eating, especially breakfast, your digestive system naturally triggers wave-like contractions that move stool through your bowel. Drinking warm beverages upon waking helps stimulate this process. Coffee helps promote bowel movement through the natural compounds it contains, regardless of caffeine content.
Squatting or using a footstool to elevate your knees above your hips straightens the passage between your rectum and anus. This reduces the effort needed to pass stools. This position also relaxes the muscle that keeps your rectum typically kinked, preventing accidental bowel movements. Consider using the toilet within a reasonable time after meals when your bowels are most active.
Singapore-Specific Dietary Solutions
Local hawker favourites require strategic modifications to support digestive health. Choose brown rice or whole grain noodles at the economy rice stalls. Add extra vegetables like kangkung, kai lan, or bitter gourd, which provide both fibre and water. Request less oil in stir-fried dishes to prevent delayed gastric emptying that can contribute to constipation.
Traditional Chinese soups offer hydration while providing soluble fibre from ingredients like lotus root, white fungus, and winter melon. Barley water, a typical local beverage, contains beta-glucan fibre that softens stools while providing anti-inflammatory benefits. Green bean soup delivers resistant starch that ferments in the colon to produce beneficial short-chain fatty acids.
Tropical fruits, available year-round, offer specific digestive benefits. Papaya contains papain enzymes that aid protein digestion and reduce transit time. Dragon fruit’s small seeds act as natural stool softeners while its mucilage content lubricates the intestinal tract. Prunes, though imported, may support digestive health. Their sorbitol content draws water into the intestines while phenolic compounds stimulate colonic contractions.
⚠️ Important Note
Sudden increases in fibre intake can worsen symptoms by causing gas and bloating, which increase intra-abdominal pressure. A healthcare professional can provide guidance on gradually increasing fibre intake over a few weeks. Simultaneously increase water intake to help prevent fibre from hardening in the intestines.
Medical Treatments That Address Both Conditions
Osmotic laxatives like lactulose and polyethene glycol (substances that help draw water into the intestines) work by pulling water into the intestinal lumen through osmosis. This softens stools without causing dependency. These medications work within several days. They can be used long-term under medical supervision. A healthcare professional will typically start with a low dose and adjust it based on your stool consistency rather than how often you go.
Topical treatments (creams or ointments applied directly to the affected area) for haemorrhoids target multiple pathways simultaneously. Preparations containing lidocaine (a numbing agent) can provide immediate pain relief. Hydrocortisone (an anti-inflammatory medication) reduces inflammation and itching. Calcium channel blockers, such as diltiazem ointment, reduce anal sphincter spasm (tightening of the muscle around the anus). This improves blood flow and promotes healing. Phlebotonics like diosmin strengthen vein walls and reduce capillary permeability (the ability of small blood vessels to leak fluid).
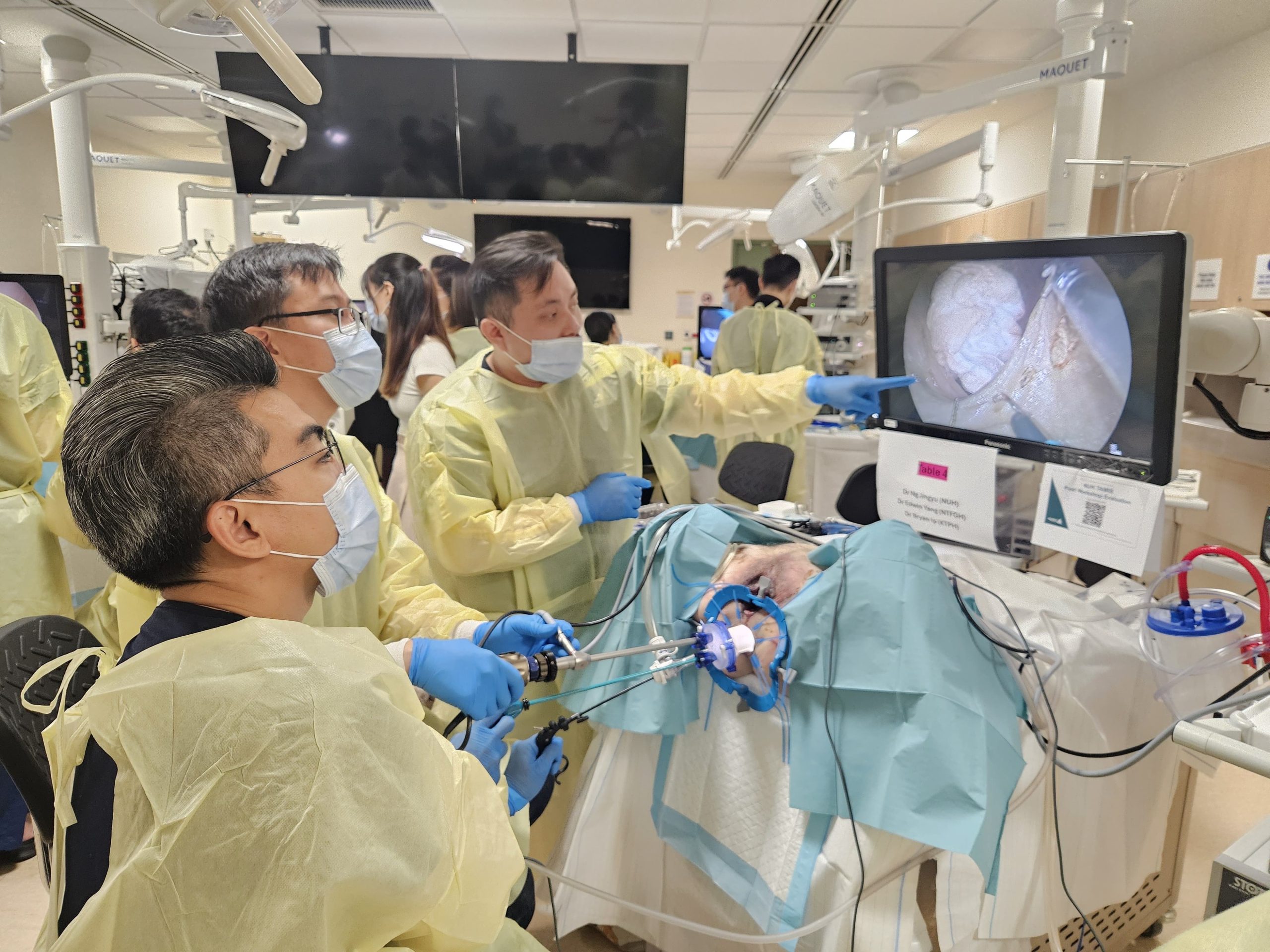
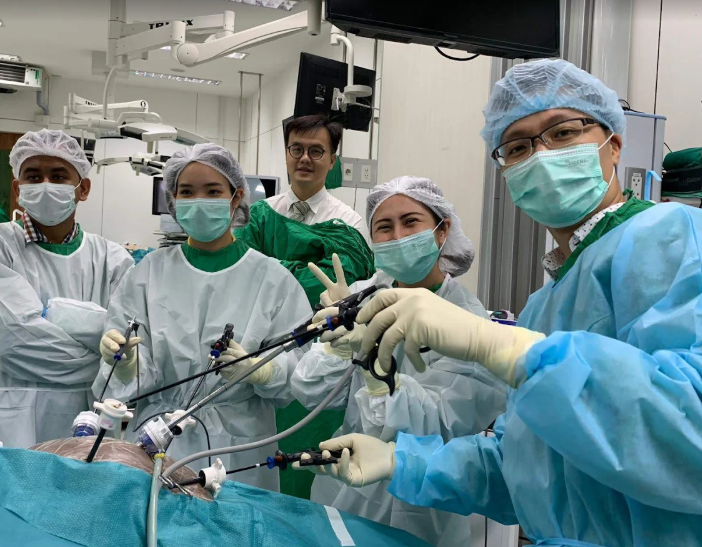
Rubber band ligation is a procedure used for Grade II-III internal haemorrhoids. It is effective in appropriately selected patients. During the procedure, a healthcare professional places small elastic bands above the dentate line (an area where pain fibres are absent). This causes the haemorrhoid to die off and fall away within several days. Multiple sessions spaced a few weeks apart may be needed for circumferential haemorrhoids (haemorrhoids that occur around the entire anal canal).
Energy-based treatments offer alternatives to traditional surgery. Haemorrhoidal artery ligation (HAL) uses Doppler ultrasound (a type of imaging technology) to identify and tie off feeding arteries. This reduces blood flow to haemorrhoids. Radiofrequency ablation uses controlled heat to create tissue changes. These changes can trigger fibrosis (scar tissue formation) and haemorrhoid shrinkage over several weeks.
Conclusion
Breaking the constipation-haemorrhoid cycle requires addressing stool consistency by gradually increasing fibre intake and maintaining adequate hydration. Maintaining Type 3-4 stools on the Bristol Stool Scale prevents straining, which worsens both conditions. Early-stage haemorrhoids respond well to conservative management, but advanced grades may require medical procedures.
If you are experiencing rectal bleeding, persistent constipation, or signs of prolapsed haemorrhoids, consult with a colorectal surgeon for appropriate evaluation and treatment.