Does anal itching wake you up at night or interfere with your daily activities? Persistent anal itching, medically termed pruritus ani, affects the perianal skin surrounding the anal opening and can signal various underlying conditions ranging from minor irritations to systemic diseases like diabetes or thyroid disorders. The condition creates a cycle where scratching damages delicate perianal skin, leading to increased irritation and more intense itching. Understanding the distinction between primary pruritus ani (idiopathic, meaning the cause is unknown) and secondary causes (where itching results from an identifiable medical condition, such as haemorrhoids, infection, or skin disorders) helps determine suitable management strategies.
Common Medical Conditions Behind Anal Itching
Haemorrhoids and Anal Fissures
Internal haemorrhoids (swollen blood vessels inside the rectum) produce mucus discharge that irritates the skin around the anus. This creates persistent moisture and itching. The mucus contains inflammatory proteins that trigger nerve endings in the sensitive anal region. External haemorrhoids (swollen blood vessels outside the anus) cause itching through direct inflammation and the formation of skin tags. These tags trap moisture and faecal matter. Haemorrhoidal tissue becomes more problematic during bowel movements, releasing additional irritants.
Anal fissures (small tears in the lining of the anus) create sharp pain when passing stool. Intense itching follows as healing begins. The body’s inflammatory response to the tear produces histamines (chemicals released during inflammation) and other mediators that stimulate itch receptors. Muscle spasms around the fissure reduce blood flow. This slows healing and prolongs the itch-scratch cycle. Chronic fissures develop thickened edges that harbour bacteria and maintain inflammation.
Dermatological Conditions
Contact dermatitis (skin inflammation caused by irritants or allergens) in the anal region results from reactions to toilet paper dyes, wet wipes, soaps, or topical medications. The thin skin around the anus, rich in blood vessels, is susceptible to irritants. Fragranced products and preservatives like methylisothiazolinone commonly trigger reactions. These persist until the offending agent is identified and eliminated.
Psoriasis (a chronic skin condition causing red, scaly patches) can affect the area around the anus in some patients with the condition elsewhere on their bodies. The characteristic silver scales and red patches extend into the fold between the buttocks, causing intense itching. Inverse psoriasis specifically targets skin folds, making the anal region particularly susceptible. The constant moisture and friction in this area exacerbate psoriatic plaques (raised, inflamed skin patches).
Lichen sclerosus (a chronic skin condition) produces white, thin patches around the anus with severe itching that worsens at night. The condition causes progressive scarring and thinning of the skin. This makes the area more vulnerable to tears and secondary infections. Women experience this condition more frequently, though men with involvement around the anus may have more severe symptoms.
Infections That Trigger Anal Itching
Fungal Infections
Candida (a type of yeast) thrives in the warm, moist environment of the perianal region, commonly in patients with diabetes or those taking antibiotics. The yeast produces enzymes that break down skin proteins. This causes inflammation and itching. Satellite lesions (small patches of infection) surrounding the main infection area can help distinguish fungal from bacterial causes. Antifungal powders may not be effective because they don’t address the underlying moisture problem.
Dermatophyte infections (tinea cruris, also known as “jock itch”) extend from the groin into the perianal area. They create a characteristic ring-like pattern. The fungus feeds on keratin (a protein) in the skin’s outer layer. It releases metabolites (waste products) that trigger immune responses and itching. Sweating and tight clothing create conditions for fungal growth.
Bacterial Infections
Streptococcal perianal dermatitis (a bacterial skin infection) presents as bright red, well-demarcated inflammation with itching. The bacteria produce toxins that directly stimulate nerve endings whilst breaking down the skin barrier. Children are more likely to develop this condition, often following streptococcal pharyngitis (strep throat). The infection requires systemic antibiotics (taken by mouth or injection) rather than topical treatment alone.
Scratching introduces staphylococcus (a type of bacteria) or other bacteria into damaged skin. This causes secondary bacterial infections. These infections produce additional inflammation. They may form small pustules (pus-filled bumps) around the anus. Methicillin-resistant Staphylococcus aureus (MRSA, a type of bacteria resistant to many antibiotics) can cause perianal infections requiring specific antibiotic selection.
Parasitic Causes
Pinworms (small, thread-like worms) migrate to the perianal area at night to lay eggs. This causes nocturnal itching. The female worm’s movements and the irritating substance in the egg adhesive trigger scratching. Children transmit pinworms through contaminated hands and surfaces. The eggs can remain viable for several weeks on bedding and clothing.
Scabies mites (tiny insects) burrow into perianal skin, though they typically affect other body areas first. The mites’ saliva, eggs, and faeces trigger allergic reactions. These reactions cause itching that intensifies after hot showers. The itching can continue for several weeks after treatment as the body clears dead mites and their waste products.
Dietary Triggers and Sensitivities
Specific foods alter stool pH and consistency. This can irritate the anal canal during passage.
Coffee increases colonic motility. It also relaxes the anal sphincter, the muscle that controls the opening of the anus. This can allow liquid stool to leak and irritate the skin around the anus. The caffeine stimulates nerve endings, heightening itch sensation. Decaffeinated coffee still contains compounds that can trigger these effects.
Citrus fruits, tomatoes, and spicy foods contain acids and capsaicin. Capsaicin is the compound that makes peppers hot. These compounds survive digestion. They activate pain and itch receptors in the anal canal during bowel movements. Chocolate contains methylxanthines, compounds similar to caffeine, that relax smooth muscle. This potentially allows stool seepage. Dairy products in lactose-intolerant individuals create loose stools. These irritate and inflame the tissues around the anus.
Alcohol causes blood vessels in haemorrhoidal tissue to expand. It also dehydrates stool, leading to straining and tissue trauma. Beer and wine contain additional compounds like histamines and sulphites. Histamines are chemicals involved in immune responses. Sulphites are preservatives. Some individuals cannot properly break down these compounds. This can lead to reactions, including anal itching.
Systemic Conditions Manifesting as Anal Itching
Diabetes mellitus creates multiple pathways to anal itching:
- Elevated glucose levels in sweat and tissues promote fungal growth
- Diabetic neuropathy alters sensation, causing abnormal itch perception
- Poor wound healing from high blood sugar allows minor trauma from scratching to persist
- Autonomic dysfunction affects anal sphincter control, leading to incontinence and moisture accumulation
Liver disease causes bile salt accumulation in skin tissues, directly activating itch receptors. Primary biliary cholangitis and primary sclerosing cholangitis are associated with severe pruritus. The itching often precedes other symptoms of liver dysfunction. Cholestyramine binds bile salts in the intestine, reducing their systemic levels and may help alleviate itching.
Inflammatory bowel disease creates anal itching through multiple mechanisms:
- Frequent diarrhoea irritates the perianal skin
- Fistulas and abscesses create chronic inflammation
- Crohn’s disease may cause perianal skin tags that trap moisture and bacteria
- Medications used to treat IBD, including mesalamine suppositories, sometimes cause contact dermatitis
Iron deficiency anaemia produces generalised pruritus that often concentrates in the anal region. The exact mechanism remains unclear but may involve altered nerve function from tissue hypoxia. Correcting the iron deficiency may gradually resolve the itching over several weeks to months.
Diagnostic Approach
Physical examination reveals specific features that guide diagnosis:
- Lichenification (thickened skin from chronic scratching) indicates ongoing irritation
- Excoriations (scratches or abrasions) suggest acute trauma
- Erythema patterns (areas of redness) distinguish fungal from bacterial causes
- Skin tags, fissures (small tears in the skin), and haemorrhoids are directly visible with appropriate positioning and lighting
- Digital rectal examination assesses sphincter tone and can identify masses or irregularities
Diagnostic tests include:
- The scotch tape test, collected first thing in the morning, can detect pinworm eggs
- Fungal cultures differentiate candida from dermatophyte infections, guiding antifungal selection
- Bacterial cultures identify specific organisms and antibiotic sensitivities
- Patch testing can reveal contact allergens when dermatitis is suspected
Specialised examinations:
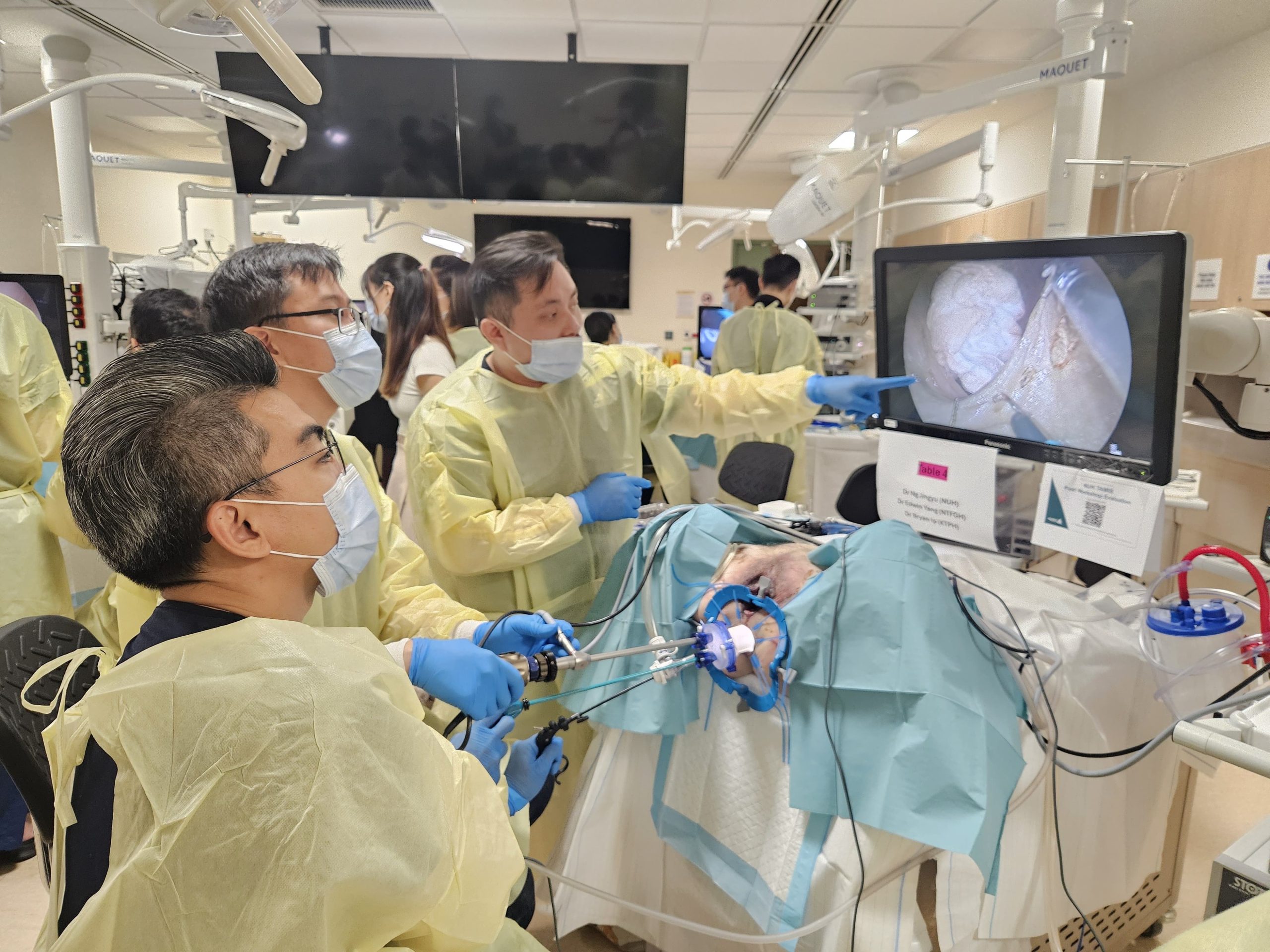
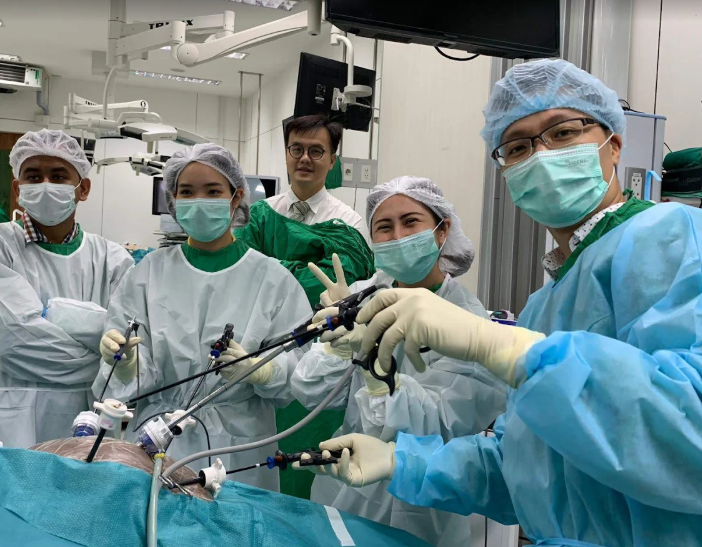
- Anoscopy visualises internal haemorrhoids, fissures, and mucosal abnormalities not visible externally
- Colonoscopy may be considered when bleeding accompanies itching or when symptoms persist despite treatment
- Biopsy of suspicious lesions can help rule out malignancy and confirm dermatological conditions like lichen sclerosus or psoriasis
Treatment Strategies
Hygiene Modifications
Gentle cleansing with water alone or pH-balanced cleansers (products designed to match the skin’s natural acidity level) helps prevent irritation from soaps and fragrances. Pat dry rather than rub to reduce mechanical trauma to inflamed skin. Cotton underwear allows air circulation whilst avoiding synthetic materials that trap moisture. Change underwear when damp from sweat to prevent maceration (softening and breakdown of skin from excessive moisture).
Barrier creams containing zinc oxide or petroleum jelly protect skin from moisture and irritants. Apply these thinly to avoid trapping moisture. Avoid products with lanolin, propylene glycol, or preservatives that commonly cause contact reactions (skin irritation or allergic responses when the skin comes into contact with certain substances).
Medical Treatments
Topical corticosteroids (anti-inflammatory creams applied directly to the skin) reduce inflammation but require careful use to prevent thinning of the skin. A healthcare professional should determine the appropriate frequency and duration of hydrocortisone use to help break the itch-scratch cycle. More potent steroids should be used only under medical supervision. Combination products with antifungals address mixed infections.
Oral antihistamines (medications that block histamine, a chemical your body releases during allergic reactions) reduce nighttime itching, improving sleep and reducing unconscious scratching. Nonsedating antihistamines provide daytime relief without drowsiness. Gabapentin or pregabalin (medications developed initially for nerve pain) treat neuropathic itch (itching caused by nerve dysfunction) when conventional treatments fail.
Injectable botulinum toxin (a purified protein that temporarily relaxes muscles) reduces anal sphincter spasm (involuntary tightening of the muscle that controls the opening of the anus) in chronic fissures, improving blood flow and healing. The treatment also decreases mucus production from internal haemorrhoids. Effects last several months, often allowing complete healing during this period.
💡 Did You Know?
The perianal region contains specialised nerve endings called C-fibres that transmit itch signals differently from pain signals. These nerves can become hypersensitised (increasingly sensitive to stimulation) through repeated stimulation. This explains why chronic anal itching may worsen over time, even when the original cause resolves.
Daily Management Techniques
Keep fingernails short and smooth to minimise skin damage from unconscious scratching during sleep. Wearing cotton gloves at night provides a physical barrier against scratching whilst allowing skin to breathe. Place a thin cotton cloth between the buttocks to absorb moisture and reduce friction during daily activities.
Establish a consistent bowel routine to minimise straining and prolonged toilet time. Limit sitting on the toilet to a short duration to prevent venous congestion in haemorrhoids (swollen blood vessels in the rectal area). Use a footstool to achieve appropriate positioning for bowel movements.
Apply cool compresses for relief during intense itching episodes. Witch hazel pads have astringent properties (which help tighten tissues) that can help reduce inflammation and dry excess moisture. Avoid applying ice directly to the skin, as this can cause thermal injury to delicate tissues.
Maintain a food diary to identify dietary triggers unique to your situation. Eliminate suspected triggers for a period, then reintroduce one at a time to confirm reactions. Common triggers vary significantly between individuals, making personal testing a practical approach.
Manage stress through regular exercise and relaxation techniques. Stress hormones (chemical messengers released during stress, such as cortisol and adrenaline) can intensify itch perception. Progressive muscle relaxation can help reduce anal sphincter tension that may contribute to symptoms.
When to Seek Professional Help
- Itching persists beyond two weeks despite hygiene modifications
- Bleeding occurs with bowel movements or wiping
- Visible lumps, bumps, or skin changes develop around the anus
- Pain accompanies the itching, especially during or after bowel movements
- Discharge of pus, mucus, or unusual fluid occurs from the anal area
- Fever or signs of spreading infection (such as increasing redness, warmth, or swelling) appear
- Nighttime symptoms disrupt sleep
- Over-the-counter treatments provide no relief after a reasonable trial period
- Changes in bowel habits (such as persistent diarrhoea, constipation, or changes in stool consistency) occur alongside itching
- You have a previous history of colorectal polyps (abnormal growths in the colon or rectum) or cancer
Commonly Asked Questions
Can stress alone cause persistent anal itching?
Stress intensifies how strongly you perceive the itch. It may trigger unconscious clenching of anal muscles, creating moisture and irritation. Whilst stress rarely causes anal itching on its own, it significantly worsens existing conditions. Managing stress through exercise, meditation, or counselling often helps reduce how symptoms feel when combined with treating the underlying cause.
Why does anal itching worsen at night?
Body temperature rises during sleep, increasing blood flow to the area around the anus and intensifying itch sensations. The absence of daytime distractions makes itching more noticeable. Certain conditions, such as pinworms (small parasitic worms), can specifically cause symptoms at night. Additionally, lying down may trap moisture in the anal area. Unconscious scratching during sleep perpetuates the cycle.
How long should I try home treatments before seeing a doctor?
Try basic hygiene measures (such as gentle cleaning and keeping the area dry) and over-the-counter treatments for up to 1 to 2 weeks. Seek immediate medical attention if any of the following develop:
- Bleeding
- Pain
- Signs of infection (such as increased redness, warmth, or pus)
Persistent symptoms beyond two weeks require professional evaluation to identify underlying conditions that won’t resolve with home care alone.
Can anal itching indicate cancer?
Whilst anal and colorectal cancers can cause itching, they are less common causes compared to haemorrhoids (swollen blood vessels in the anal area), skin conditions, and infections. Cancer-related itching often accompanies other symptoms, such as bleeding, pain, or lumps you can feel. Any persistent anal symptoms warrant evaluation. Most cases have benign, treatable causes.
Is anal itching contagious?
The itching itself isn’t contagious. Specific underlying causes spread between people. Pinworms (small parasitic worms) are transmitted easily through contaminated surfaces and close contact. Fungal and bacterial infections may spread through shared towels or direct contact. Sexually transmitted infections (STIs) affecting the anal area require partner notification and treatment.
Next Steps
Most cases of persistent anal itching respond to proper hygiene modifications and treatment of underlying causes. Document symptoms, triggers, and treatment responses to guide medical evaluation when needed. Early intervention prevents complications and breaks the itch-scratch cycle.
If you’re experiencing persistent anal itching, bleeding with bowel movements, or nighttime symptoms disrupting sleep, consult with a colorectal surgeon for specialised evaluation and treatment.