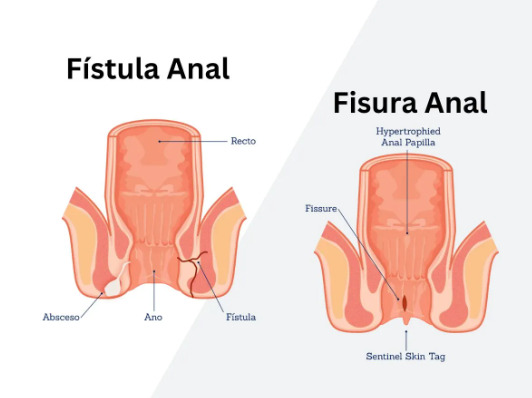
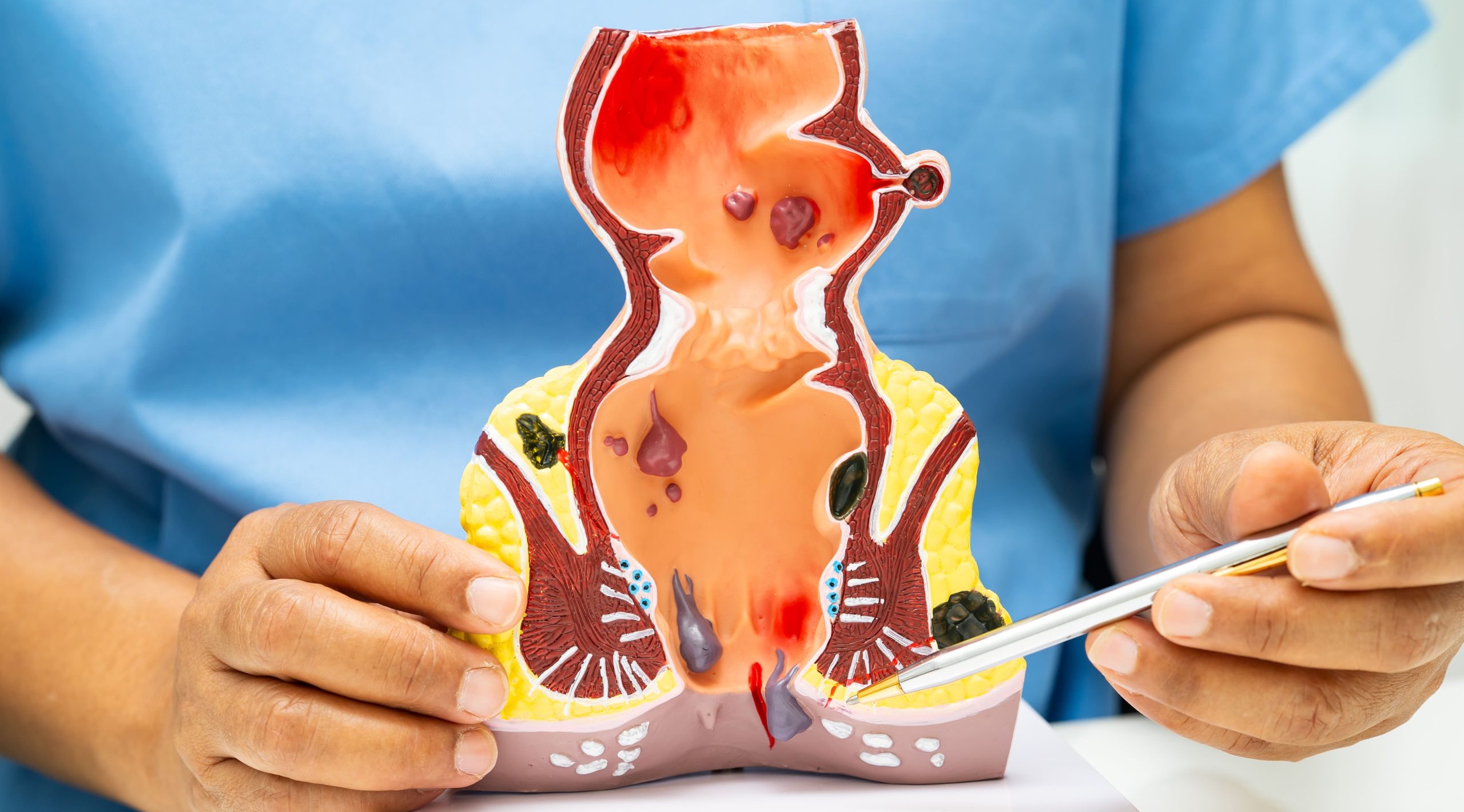
Do you experience persistent drainage near your anus that won’t heal with standard treatments? An anal fistula creates an abnormal tunnel between the anal canal and the skin near the anus, causing persistent drainage, discomfort, and recurring infections. Women face unique challenges with this condition due to anatomical differences, childbirth-related factors, and the proximity of reproductive structures. The tunnel typically develops after an anal abscess fails to heal properly, with pus finding an alternative drainage path through surrounding tissue.
Fistulas in women often connect to the vaginal area (rectovaginal fistulas) or develop following obstetric trauma, creating additional complexity in diagnosis and treatment. The condition differs from hemorrhoids or anal fissures – while those affect surface tissues, fistulas penetrate deeper, creating a complete tract between internal and external surfaces. Without appropriate surgical intervention, anal fistulas rarely heal spontaneously and frequently lead to recurring abscesses and progressive tissue damage.
Recognizing Anal Fistula Symptoms
Persistent drainage from an opening near the anus marks the primary symptom of anal fistula in women. This drainage appears as pus, blood, or fecal matter on underwear, requiring frequent pad changes throughout the day. The external opening resembles a small hole or raised bump on the skin, often surrounded by inflamed, reddened tissue.
Pain patterns vary based on fistula location and complexity. Simple, low fistulas cause mild discomfort during bowel movements, while complex or high fistulas create constant throbbing pain that intensifies when sitting. The pain typically differs from hemorrhoid discomfort – fistula pain persists between bowel movements and worsens with pressure or movement.
Skin irritation develops from constant moisture and discharge around the anal area. The affected skin becomes raw, itchy, and develops a burning sensation that topical creams cannot resolve. Unlike simple dermatitis, this irritation stems from internal drainage and requires addressing the underlying fistula.
Recurring abscesses signal active infection within the fistula tract. These abscesses form when the internal opening becomes blocked, causing pus accumulation that eventually breaks through the skin. Each abscess episode creates additional scarring and potentially new fistula branches.
Women with rectovaginal fistulas experience vaginal discharge of gas or stool, particularly during bowel movements. This symptom significantly impacts quality of life and requires surgical planning to preserve sphincter function and vaginal integrity.
Causes Specific to Women
Childbirth trauma accounts for many anal fistulas in women, particularly after prolonged labor, large babies, or instrumental deliveries. Third and fourth-degree perineal tears that extend into the anal sphincter create vulnerability to fistula formation, especially if initial repair experiences complications or infection. Episiotomies that extend beyond intended boundaries or heal poorly also increase fistula risk.
Inflammatory bowel disease affects women differently than men, with hormonal fluctuations influencing disease activity. Crohn’s disease particularly predisposes women to complex perianal fistulas that may connect to the vagina or involve multiple tracts. These fistulas require coordinated management between colorectal surgeons and gastroenterologists.
Previous anorectal surgeries, including hemorrhoidectomy or anal fissure procedures, occasionally lead to fistula development when healing complications occur. Radiation therapy for gynecological cancers weakens tissue integrity in the pelvic region, creating conditions where fistulas develop months or years after treatment completion.
Bartholin’s gland abscesses, though primarily gynecological, can extend toward the anal area and create complex fistula patterns. These cases require careful evaluation to determine the primary origin and appropriate surgical approach.
Diagnostic Methods
Physical examination reveals the external fistula opening and helps determine tract direction through gentle probing. Digital rectal examination identifies the internal opening location and assesses sphincter muscle integrity. In women, vaginal examination checks for rectovaginal connections or involvement of gynecological structures.
Anoscopy allows direct visualization of the internal opening within the anal canal. The procedure uses a small, lighted scope to examine the lower rectum and identify inflammation, scarring, or multiple internal openings that suggest complex fistula anatomy.
MRI pelvis provides detailed imaging of fistula tracts, particularly for complex cases involving multiple branches or high fistulas near the sphincter muscles. The scan reveals tract direction, abscess pockets, and relationships to pelvic organs without radiation exposure. Contrast enhancement improves visualization of active inflammation within fistula walls.
Endoanal ultrasound uses a specialized probe to create detailed images of anal sphincter muscles and fistula tracts. This technique identifies internal openings and assesses sphincter defects from previous trauma or surgery. The real-time imaging helps surgeons plan procedures that preserve continence.
Examination under anesthesia becomes necessary when pain prevents thorough office evaluation or when complex anatomy requires detailed assessment. Surgeons can probe the fistula tract, inject dye to trace connections, and perform simultaneous drainage of abscesses if present.
Surgical Treatment Approaches
Fistulotomy
Fistulotomy is a treatment option for simple, low fistulas that involve minimal sphincter muscle. The surgeon opens the entire fistula tract, converting the tunnel into a groove that heals from the bottom up. Recovery takes 4-6 weeks, with daily wound care supporting proper healing progression.
The procedure can achieve healing in simple fistulas but requires careful patient selection. Women with anterior fistulas face higher continence risks due to shorter sphincter length in this region. Post-operative care includes sitz baths, stool softeners, and gradual return to normal activities.
Seton Placement
Seton techniques use surgical thread or elastic bands placed through the fistula tract to promote gradual healing while preserving sphincter function. Cutting setons slowly divide the muscle over several weeks, allowing fibrosis to maintain continence. Draining setons control infection without dividing muscle, preparing complex fistulas for definitive repair.
Women may benefit from seton placement when fistulas involve significant sphincter muscle or when acute inflammation requires initial control. The technique allows staged treatment, reducing the risk of incontinence while achieving fistula resolution. Seton adjustment occurs in clinic every 2-3 weeks until adequate drainage or muscle division occurs.
Advancement Flap Procedures
Endorectal advancement flaps mobilize healthy rectal tissue to cover the internal fistula opening after tract excision. This technique preserves sphincter integrity while achieving fistula closure, particularly valuable for women with anterior fistulas or previous obstetric injuries.
The procedure involves creating a tongue-shaped flap of rectal wall, excising the fistula tract, and suturing the flap over the internal opening. Success depends on adequate blood supply to the flap and absence of active infection. Recovery requires 6-8 weeks of modified activity to prevent flap disruption.
LIFT Procedure
Ligation of Intersphincteric Fistula Tract (LIFT) approaches the fistula through the intersphincteric plane, preserving external sphincter function entirely. The surgeon identifies and divides the fistula tract between internal and external sphincter muscles, then removes infected tissue from both openings.
This technique suits women with trans-sphincteric fistulas who prioritize continence preservation. The procedure combines healing rates with minimal functional impact, though complex fistulas may require additional interventions. Post-operative recovery involves wound care at both the intersphincteric incision and external opening sites.
Post-Surgical Recovery
Week 1-2 focuses on pain management and preventing constipation that could disrupt surgical repairs. Sitz baths three times daily reduce inflammation and promote healing. Wound packing changes occur daily for open procedures, with gradual reduction as granulation tissue forms. Antibiotics continue if infection signs persist.
Week 3-4 brings decreased drainage and improved comfort during bowel movements. Dietary fiber supplements maintain soft, formed stools that pass without straining. Physical activity gradually increases, though heavy lifting and strenuous exercise remain restricted. Sexual activity may resume after surgeon clearance, usually around week 4 for simple repairs.
Week 5-8 sees continued wound contraction and epithelialization for open wounds. Advancement flap patients experience minimal external healing needs but require careful monitoring for internal healing. Return to full activities, including exercise and swimming, occurs once external wounds close completely.
Long-term recovery involves surveillance for fistula recurrence. Maintaining bowel regularity through diet and hydration reduces strain on healing tissues. Pelvic floor physiotherapy helps restore muscle function, especially for women with previous obstetric trauma.
Commonly Asked Questions
How does pregnancy affect anal fistula treatment?
Pregnancy typically delays definitive surgical treatment until after delivery, with seton drainage providing symptom control during gestation. Simple fistulotomy may proceed during second trimester if symptoms impact quality of life. Post-partum treatment planning considers breastfeeding status and potential future pregnancies when selecting surgical approaches.
Can anal fistulas affect fertility or future pregnancies?
Anal fistulas themselves don’t impact fertility, though complex fistulas involving reproductive organs may require careful surgical planning. Treatment before pregnancy can reduce infection risks and improve comfort during gestation. Previous fistula surgery doesn’t contraindicate vaginal delivery unless extensive sphincter reconstruction was performed.
What’s the difference between hemorrhoids and anal fistulas?
Hemorrhoids involve swollen blood vessels that cause bleeding, protrusion, and discomfort primarily during bowel movements. Anal fistulas create persistent drainage through an abnormal tunnel, with symptoms continuing between bowel movements. Hemorrhoids may respond to conservative treatment, while fistulas typically require surgical intervention for resolution.
How long before returning to work after fistula surgery?
Desk work typically resumes within 1-2 weeks for simple fistulotomy, while physical jobs may require 3-4 weeks recovery. Complex procedures involving advancement flaps or multiple tracts may need 4-6 weeks before returning to work duties. Individual healing rates and job requirements determine specific return-to-work timing. Consult your healthcare professional for personalized guidance.
Do anal fistulas always require surgery?
Anal fistulas rarely heal without surgical intervention, as the epithelialized tract prevents spontaneous closure. Antibiotics may temporarily reduce symptoms but don’t achieve permanent healing. Delaying surgery may lead to abscess recurrence, tract complexity increase, and potential sphincter damage from repeated infections.
Conclusion
Early surgical intervention prevents fistula complexity and reduces sphincter damage risk. Current surgical techniques offer various approaches tailored to individual anatomy and patient factors, with preservation of continence being a primary consideration for women.
If you’re experiencing persistent anal drainage, recurring abscesses, or connections between anal and vaginal areas, a MOH-accredited colorectal surgeon can provide comprehensive evaluation and personalized treatment options.