Recovery Timeline After Anal Fistula Surgery
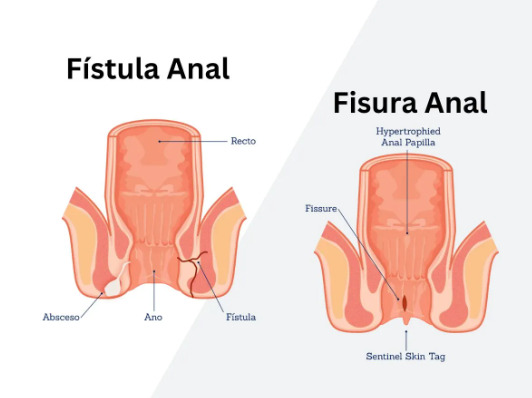
What determines how quickly you’ll heal from anal fistula surgery? Recovery follows predictable patterns, though individual healing varies based on fistula complexity, surgical technique, and overall health. Simple fistulotomy procedures involve shorter recovery than complex procedures like LIFT (ligation of intersphincteric fistula tract) or advancement flap repairs. The location and depth of the fistula tract directly influences both surgical approach and healing duration.
Recovery divides into distinct phases:
- Immediate post-operative (first 48 hours)
- Early recovery (weeks 1-2)
- Wound maturation (weeks 3-6)
- Complete healing (6-12 weeks)
Pain typically peaks during the first bowel movement post-surgery, then gradually decreases over 7-10 days. Wound drainage continues for several weeks as the surgical site heals from inside outward.
The surgeon’s technique affects recovery significantly. Fistulotomy creates an open wound requiring daily dressing changes, while procedures preserving the sphincter muscle may involve internal sutures and different care protocols.
First 48 Hours Post-Surgery
Immediate post-operative care focuses on pain control and preventing complications. You’ll receive prescription pain medication, typically combining paracetamol with stronger analgesics for breakthrough pain. Local anaesthetic effects wear off within 4-6 hours, making proactive pain management important before discomfort intensifies.
Consult your healthcare professional regarding stool softeners post-surgery. Options may include docusate sodium or lactulose to prevent straining. Warm sitz baths before bowel movements can help relax the sphincter muscles, reducing pain. Sitting in warm water for 10-15 minutes may also help afterward, cleansing the area while providing pain relief.
Bleeding may appear during initial bowel movements. Fresh red blood on toilet paper or dripping into the bowl occurs commonly. Gentle pressure with gauze for 5-10 minutes may help if bleeding seems excessive. Dark blood clots or bleeding soaking through multiple pads within an hour requires immediate medical attention.
💡 Did You Know?
The anal area contains dense nerve endings, making post-surgical pain feel more intense than similar wounds elsewhere. This concentrated innervation actually promotes faster healing through increased blood flow.
A healthcare professional can advise on appropriate fiber intake through fruits, vegetables, and whole grains. Adequate water intake helps maintain soft stools. Avoiding spicy foods, alcohol, and caffeine may help prevent irritation of the surgical site. Small, frequent meals may help prevent constipation better than three large meals.
Week 1-2: Early Recovery Phase
Pain patterns change during early recovery. Sharp, stabbing pain during bowel movements gradually transforms into dull aching between movements. Many patients reduce prescription pain medication to nighttime use only by day 5-7, managing daytime discomfort with paracetamol alone. Ice packs applied for 10 minutes several times daily provide additional relief without medication side effects.
Wound drainage remains substantial during this period. Yellow or blood-tinged discharge soaks through 3-4 gauze pads daily initially, decreasing to 1-2 pads by week two. This drainage indicates normal healing as the fistula tract closes from its deepest point outward. Foul-smelling discharge or increased drainage volume after initial improvement suggests infection requiring antibiotics.
Daily wound care prevents infection and promotes healing. After each bowel movement:
- Rinse the area with warm water using a handheld shower or sitz bath
- Pat dry gently with soft towels (avoid rubbing)
- Apply prescribed antibiotic ointment if directed
- Place clean gauze between buttocks to absorb drainage
- Change gauze whenever soaked through, minimum 3-4 times daily
Return to activities happens gradually. Walking short distances multiple times daily prevents blood clots and promotes circulation. Avoid sitting directly on the surgical site – use a donut cushion or lie on your side when resting. Many patients return to desk work after 7-10 days, though standing frequently prevents pressure buildup on the healing wound.
⚠️ Important Note
Never use wet wipes containing alcohol or fragrance on surgical wounds. These chemicals delay healing and increase infection risk. Plain water or saline solution provides safest cleansing.
Week 3-6: Wound Maturation
Healing becomes visible during weeks 3-6. The surgical wound contracts noticeably, with granulation tissue (pink, bumpy new tissue) filling the defect. Drainage decreases to slight spotting on gauze, though temporary increases occur after physical activity or constipation episodes. Pain transforms into occasional twinges or pulling sensations as scar tissue forms.
Physical activity gradually increases during this phase. Light exercise like walking may promote healing through improved circulation. Swimming pools remain off-limits until complete wound closure, typically 6-8 weeks post-surgery. Gym activities resume progressively – start with upper body exercises, adding lower body work as comfort allows. Sexual activity typically resumes after 4-6 weeks, though positions avoiding direct pressure on the healing area work better initially.
Scar tissue formation affects bowel habits temporarily. The developing scar tissue feels firm and may cause mild narrowing sensations during bowel movements. This improves as tissue softens over subsequent weeks. Continuing stool softeners through week 6 may help prevent re-injury from straining. Some patients experience temporary urgency or minor incontinence to gas as sphincter muscles recover from surgical trauma.
Diet normalization occurs gradually. Reintroduce previously restricted foods one at a time, monitoring for irritation. Spicy foods often remain problematic through week 8-10. Maintaining high fiber intake may reduce future fistula risk by preventing constipation and anal trauma. Probiotic supplements may support digestive health during antibiotic recovery.
Long-term Healing Expectations
Complete anal fistula surgery recovery extends beyond wound closure. While surface healing completes by 6-8 weeks for simple fistulas, deep tissue remodeling continues for 3-6 months. Complex fistulas involving muscle repair or advancement flaps require 10-12 weeks for initial healing, with strength returning gradually over 6 months.
Scar tissue evolution affects long-term comfort. Initial firm, sensitive scars soften progressively through massage and normal stretching during bowel movements. Vitamin E oil or silicone-based scar treatments applied after week 8 may improve scar flexibility. Occasional pulling sensations or weather-related aching in the scar area persist for some patients up to one year post-surgery.
✅ Quick Tip
Keeping a recovery journal tracking pain levels, drainage amounts, and bowel habits helps identify healing patterns and potential complications.
Follow-up appointments monitor healing progress and identify complications. A surgeon examines the wound at 2 weeks, 6 weeks, and 3 months post-operatively. These visits assess wound closure, sphincter function, and signs of fistula recurrence. Digital rectal examination or anoscopy during these visits ensures internal healing matches external appearance.
Recurrence signs require immediate attention. New drainage from the surgical site after healing, perianal swelling, or return of pre-surgical symptoms suggests fistula recurrence. Early intervention for recurrence improves outcomes. Regular colorectal screening continues indefinitely, as previous fistula increases future risk.
Managing Complications
Post-surgical infections occur despite proper wound care. Temperature above 38.5°C, increasing pain after initial improvement, or purulent discharge indicates infection. Oral antibiotics typically resolve superficial infections within 48-72 hours. Deep infections may require surgical drainage or intravenous antibiotics.
Delayed wound healing affects certain patients disproportionately. Diabetes, smoking, and immunosuppression slow tissue repair. These patients require extended wound care, possibly 12-16 weeks for complete closure. Hyperbaric oxygen therapy or vacuum-assisted closure devices may accelerate healing in resistant cases.
Fecal incontinence ranges from minor gas leakage to loss of solid stool control. Minor incontinence affects some patients temporarily, resolving as swelling decreases and muscles strengthen. Persistent incontinence beyond 3 months requires specialized evaluation. Pelvic floor physiotherapy strengthens sphincter muscles through targeted exercises. Biofeedback training improves muscle coordination and sensation.
Anal stenosis (narrowing) develops rarely but requires prompt treatment. Progressive difficulty passing stool or pencil-thin stools suggest stenosis. Daily anal dilators used for several weeks usually restore normal caliber. Severe stenosis may require surgical revision under anesthesia.
What Our Colorectal Surgeon Says
Post-operative wound care determines healing quality more than surgical technique. Patients maintaining meticulous hygiene and following dietary recommendations consistently achieve better outcomes. The psychological impact of anal surgery often exceeds physical discomfort – understanding normal healing patterns reduces anxiety significantly.
Choosing between different surgical approaches involves careful risk-benefit analysis. Simpler procedures offer faster recovery but higher recurrence rates. Complex sphincter-preserving techniques require longer healing but maintain continence better. A surgeon can tailor the approach based on fistula anatomy, previous surgeries, and continence status.
Patient compliance with post-operative instructions directly correlates with success rates. Missing sitz baths, stopping stool softeners prematurely, or returning to strenuous activity too quickly increases complications. The investment in proper recovery pays dividends through reduced recurrence risk and better long-term function.
Putting This Into Practice
- Prepare your recovery space before surgery: Set up a sitz bath in your bathroom, stock gauze pads and prescribed ointments within easy reach of the toilet, and arrange cushions in resting areas to avoid direct pressure on the surgical site.
- Create a bowel movement routine: Take stool softeners at consistent times daily, drink warm liquids 30 minutes before typical bowel movement times to stimulate natural reflexes, and avoid delaying the urge to defecate as this hardens stool.
- Track your healing progress: Photograph the wound weekly (using a mirror or asking a trusted person) to document healing progression, record drainage amounts and characteristics to identify abnormal patterns early, and note pain levels at consistent times daily using a 1-10 scale.
- Maintain wound hygiene systematically: Shower after every bowel movement when possible, or use a portable bidet for thorough cleansing when away from home. Keep travel-sized wound care supplies in your car, office, and bag for unexpected needs.
- Build activity gradually: Increase walking distance gradually every few days after week one, add one new physical activity weekly after week 3, monitoring for increased drainage or discomfort, and plan return to full activities based on your specific healing rate rather than arbitrary timelines.
When to Seek Professional Help
- Fever above 38.5°C persisting more than 24 hours
- Bleeding requiring pad changes more than once hourly
- Severe pain uncontrolled by prescribed medication
- Foul-smelling discharge different from normal drainage
- Inability to pass stool or gas for more than 2 days
- New lump or swelling near the surgical site
- Drainage restarting after apparent healing
- Progressive difficulty with bowel movements
- Loss of bowel control beyond minor gas leakage after 6 weeks
- Wound edges separating or deepening instead of closing
Commonly Asked Questions
When can I return to work after anal fistula surgery?
Desk-based work typically resumes after 7-10 days with cushion support and frequent position changes. Physical labor requiring lifting, prolonged standing, or straining should wait 3-4 weeks minimum. Healthcare workers exposed to infection risk may need 2 weeks for adequate wound closure before patient contact resumes.
How do I know if my wound is infected versus normal healing?
Normal drainage appears yellow-white or blood-tinged without odor, decreasing daily after the first week. Infection produces thick, foul-smelling discharge, increasing pain after initial improvement, and surrounding skin redness extending beyond 1cm from wound edges. Fever accompanies surgical site infections.
Can I prevent fistula recurrence after surgery?
Maintaining soft, formed stools through dietary modification may help reduce recurrence risk. Address underlying conditions like Crohn’s disease with appropriate medical therapy. Avoid anal trauma from aggressive wiping or insertion of foreign objects. Regular colorectal follow-up identifies early recurrence when treatment options may be simpler.
Why does my first bowel movement hurt so much despite pain medication?
The first bowel movement stretches healing tissue for the first time, activating pain receptors medication cannot completely block. Sitz baths, timing of pain medication 30-45 minutes before bowel movements, and breathing exercises during passage may help minimize discomfort.
When will the drainage completely stop?
Simple fistulotomy drainage typically stops by week 4-6. Complex repairs may drain minimally for 8-10 weeks. Occasional spotting during healing is normal, especially after physical activity. Persistent daily drainage beyond 12 weeks warrants re-evaluation for incomplete healing or recurrence.
Conclusion
Successful recovery requires systematic wound care and gradual activity progression. Most patients achieve complete healing within 6-12 weeks. Follow surgeon instructions while monitoring for complications.
If you are experiencing persistent anal pain, drainage, or bleeding, a colorectal surgeon can evaluate your symptoms and discuss treatment options.