The body’s immune system mistakenly targets healthy bowel tissue, causing inflammation.
Ulcerative Colitis Singapore
Ulcerative colitis is a chronic inflammatory bowel disease affecting the large intestine (colon) and rectum. It causes inflammation and small ulcers (open sores) to develop along the inner lining of the bowel, leading to recurring symptoms. The condition typically begins in the rectum and can spread continuously along the colon, often involving cycles of remission (symptom-free periods) and flare-ups.


Symptoms of Ulcerative Colitis
Common signs of ulcerative colitis include:
- Bloody diarrhoea: Loose, frequent bowel movements containing blood or mucus.
- Abdominal pain and cramping: Discomfort or sharp pains in the lower abdomen, particularly on the left side, which may intensify before bowel movements.
- Urgency: A sudden, strong need to use the toilet that can be difficult to control or delay.
- Incomplete bowel emptying: A persistent feeling that the bowel hasn’t been fully emptied after using the toilet.
- Fatigue: Ongoing tiredness and low energy levels that may develop from blood loss, poor nutrient absorption, or the body’s inflammatory response.
- Unintentional weight loss: Weight loss due to decreased appetite, poor nutrient absorption, or frequent diarrhoea.
- Fever during flare-ups: Raised body temperature that may occur when other symptoms worsen.
Causes and Risk Factors of Ulcerative Colitis
Several factors can increase the risk of ulcerative colitis:
Immune system response
Genetic factors
Having a family member with ulcerative colitis or another inflammatory bowel condition increases the likelihood of developing the condition.
Age at onset
The condition most commonly develops between ages 15 and 30, though it can occur at any age.
Environmental triggers
Certain factors such as stress, diet changes, or infections may trigger symptoms in people who are already predisposed to the condition.
Types of Ulcerative Colitis
Ulcerative colitis is classified based on the location and extent of inflammation within the large intestine.
Proctitis
Inflammation limited to the rectum, often causing rectal bleeding and pain but typically fewer bowel movements.
Left-sided colitis
Inflammation extends from the rectum up to the left side of the colon, causing bloody diarrhoea and cramping on the left side of the abdomen.
Extensive colitis (pancolitis)
Inflammation affects most or all of the colon, often causing more severe symptoms including frequent bloody diarrhoea, abdominal pain, and fatigue.
Diagnostic Methods
Diagnosing ulcerative colitis requires a combination of tests to examine the bowel and rule out other conditions with similar symptoms.
- Medical History: Your bowel habits, dietary patterns, family history, and any past medical issues or surgeries that may influence bowel health will be discussed.
- Physical Examination: A thorough physical examination helps identify signs of inflammation, assesses abdominal tenderness, and evaluates overall bowel function.
- Colonoscopy: A thin, flexible tube with a camera is inserted through the rectum to examine the entire colon, allowing direct visualisation of inflammation and ulcers.
- CT scan: Cross-sectional imaging that can show the thickness of the bowel wall and identify complications such as perforation or abscesses.
- Stool samples: Testing of bowel movements to rule out infections and check for blood or inflammatory markers.
Ulcerative Colitis Treatment in Singapore
Non-Surgical Treatment
Medical management focuses on reducing inflammation and controlling symptoms to help achieve and maintain remission.
- Anti-inflammatory medications: Drugs such as aminosalicylates help reduce inflammation in the bowel lining and are often used for mild to moderate symptoms.
- Nutritional support: Dietary modifications and supplements to address nutritional deficiencies and support overall health during treatment.
Surgical Treatment
Surgery may be recommended when medical treatments are no longer controlling symptoms or when complications develop.
- Total colectomy with ileostomy: Complete removal of the colon with creation of an opening in the abdominal wall for waste elimination through a bag system.
- Restorative proctocolectomy (J-pouch surgery): Removal of the colon and rectum with creation of an internal pouch from the small intestine, allowing bowel movements through the original opening.
- Subtotal colectomy: Removal of most of the colon while preserving the rectum, which may be appropriate in certain circumstances.
Are Your Symptoms Affecting Your Quality of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Prevention and Management
While ulcerative colitis cannot be prevented, certain lifestyle modifications may help reduce flare-up frequency and severity. Maintaining a food diary can help identify trigger foods that worsen symptoms, though dietary triggers vary between individuals. Regular exercise, stress management techniques, and adequate sleep may support overall bowel health. Taking prescribed medications consistently, even during symptom-free periods, helps prevent symptom recurrence and reduces complication risk.
When to See a Colorectal Surgeon
Prompt consultation with a colorectal surgeon in Singapore is recommended if you have ulcerative colitis and experience any of the following:
- Persistent or worsening symptoms despite ongoing medical treatment
- Severe rectal bleeding or significant blood in your stools
- Intense abdominal pain or sudden increase in cramping
- Unintentional and ongoing weight loss despite efforts to maintain nutrition
- Frequent urgency or loss of bowel control severely impacting daily life
- Signs of complications, such as high fever, chills, or symptoms suggesting bowel obstruction or perforation
Frequently Asked Questions
Can ulcerative colitis lead to bowel cancer?
Long-standing ulcerative colitis does increase the risk of developing colorectal cancer, particularly when the entire colon is affected. Regular surveillance colonoscopies are recommended to monitor for early changes.
Will I need surgery if I have ulcerative colitis?
Most people with ulcerative colitis can manage their condition with medication alone. Surgery is typically considered when medical treatments fail to control symptoms or when complications such as severe bleeding or perforation occur.
Can pregnancy affect ulcerative colitis symptoms?
Pregnancy outcomes are generally good for women with ulcerative colitis, particularly when the condition is in remission before conception. Some women experience improved symptoms during pregnancy, while others may have flare-ups.
How often will I need follow-up appointments?
The frequency of appointments depends on your symptom severity and treatment response. During active flare-ups, more frequent monitoring may be needed, while stable patients may require check-ups every few months to annually.
Partnered Programmes & Insurance Plans
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.

















contact us
Please leave us a message and our friendly clinic staff will get back to you as soon as possible. For urgent or same day appointments, kindly call the clinic to arrange an appointment.
Our Clinic Locations
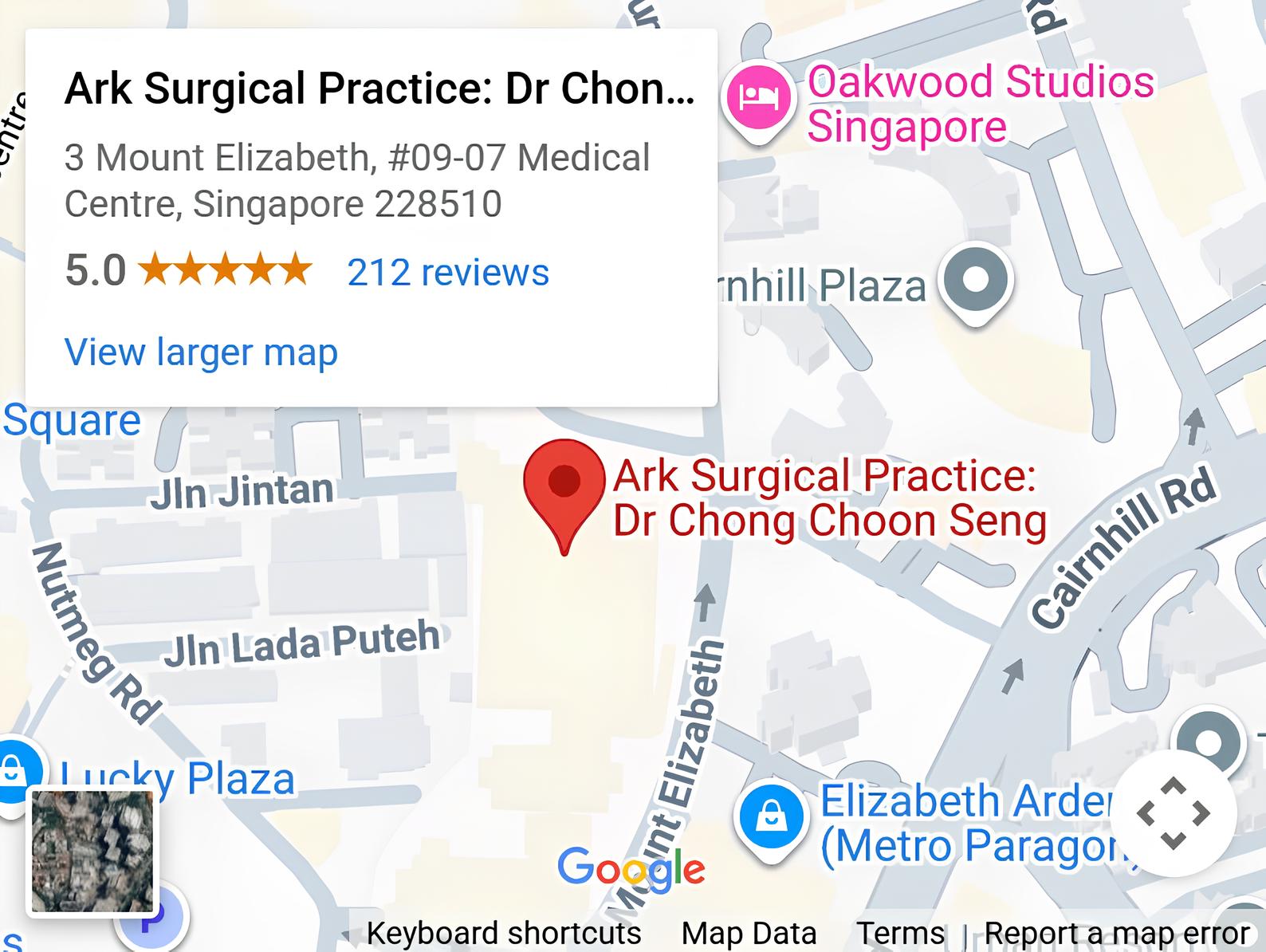
Ark Surgical Practice – Mount Elizabeth Medical Centre
3 Mount Elizabeth, #09-07
Singapore 228510
Monday to Friday: 9am – 5pm
Saturday: 9am – 12:30pm
Sunday & Public Holidays: Closed
Ark Surgical Practice – Mount Alvernia Hospital
820 Thomson Road,
Mount Alvernia Hospital, #06-52,
Medical Centre D, Singapore 574623
Wednesday: 9am – 12:30pm
Thursday: 2pm – 5pm