- Biliary Colic: This causes pain in the upper right or middle abdomen that may radiate to the back or right shoulder. The pain typically occurs after eating fatty meals and can last from 30 minutes to several hours.
- Jaundice: When gallstones block the common bile duct, bile cannot flow properly into the intestine, causing yellowing of the skin and whites of the eyes. This occurs due to increased bilirubin levels in the bloodstream.
- Nausea and Vomiting: These symptoms often accompany gallbladder pain during a gallstone attack. They result from the body’s response to inflammation and digestive disruption caused by bile flow obstruction.
- Fever and Chills: These symptoms may indicate an infection such as cholecystitis (gallbladder inflammation) or cholangitis (bile duct infection). They occur when gallstones completely block bile flow, creating an environment where bacteria can multiply.
- Digestive Disturbances: Some people experience bloating, gas, and indigestion after meals. These symptoms occur when bile flow is disrupted, affecting the digestion of fats and causing discomfort.
- Pancreatitis: Inflammation of the pancreas can develop if a gallstone blocks the pancreatic duct. This results in severe upper abdominal pain that spreads to the back, as well as nausea and vomiting.
Gallstones Treatment in Singapore
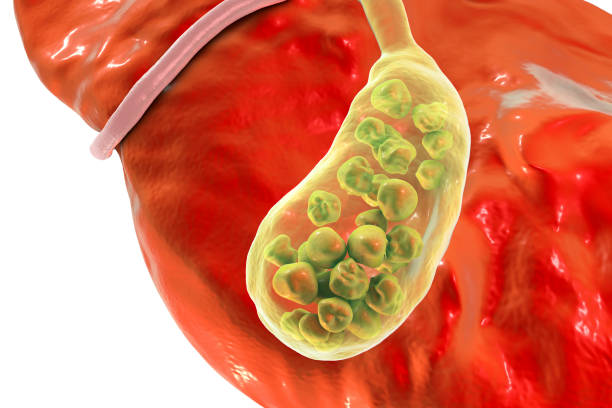
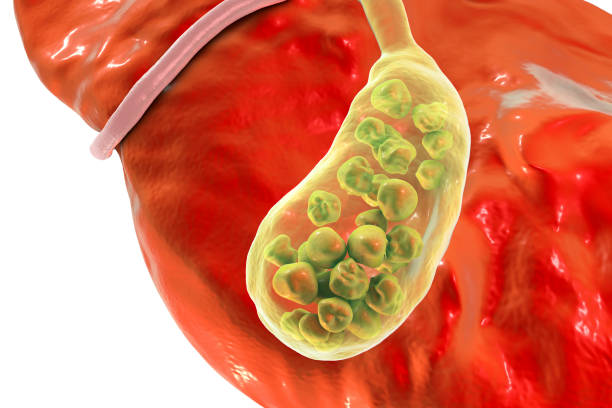
Gallstones are hard deposits that form in the gallbladder, a small organ located beneath the liver. These deposits develop when substances in bile, primarily cholesterol and bilirubin, crystallise and form solid particles. Gallstones can vary in size from tiny grains to larger stones measuring several centimetres. They can occur as a single stone or as multiple stones within the gallbladder. When gallstones block the bile ducts, they can cause pain, inflammation, and other complications that affect digestive health.
Symptoms of Gallstones
Gallstones may cause various symptoms when they block bile ducts or cause inflammation within the gallbladder or surrounding structures.
Causes and Risk Factors
Gallstones form when bile components become imbalanced, creating conditions favourable for crystallisation and stone formation.
Cholesterol Concentration
Most gallstones consist primarily of cholesterol. They form when the liver produces bile with too much cholesterol for the bile salts to dissolve, leading to crystal formation and eventual stone development.
Bile Pigment Imbalance
Bilirubin stones develop when bile contains excess bilirubin, often due to liver conditions or blood disorders. These stones form when red blood cells break down abnormally or in larger quantities. This can happen in patients with hemolytic anaemia or abnormal blood disorders with increase in red blood cell destruction.
Gallbladder Emptying Problems
Incomplete or infrequent emptying of the gallbladder can cause bile to become concentrated. This stasis creates conditions where substances can precipitate and form stones over time.
Age and Gender
The risk increases with age, particularly after 40, and women are twice as likely to develop gallstones as men. This difference relates to hormonal factors, especially oestrogen, which increases cholesterol in bile.
Genetic Factors
Certain genetic factors affect bile composition and gallbladder function, predisposing some individuals to stone formation.
Obesity
Excess weight increases cholesterol production by the liver and alters bile composition. People with obesity have higher cholesterol levels in bile, increasing the risk of stone formation.
Dietary Factors
Diets high in cholesterol and fat and low in fibre may contribute to gallstone formation. These dietary patterns alter bile composition, making it more likely to form stones.
Medications
Certain drugs, such as oral contraceptives, hormone replacement therapy, and cholesterol-lowering medications, can affect bile composition. These medications can increase cholesterol levels in the bile or alter gallbladder function.
Diagnostic Methods
Abdominal Ultrasound
This is the primary imaging test for diagnosing gallstones. Sound waves create images of the gallbladder, revealing stones as well as signs of inflammation or biliary obstruction. The procedure is non-invasive, painless, and does not involve radiation exposure, making it suitable for pregnant women and those requiring repeated examinations.
CT Scan
Computed tomography provides detailed cross-sectional images of the abdomen, showing gallstones and complications such as pancreatitis or cholecystitis. CT scans can detect stones that may be missed by ultrasound, particularly in the bile ducts, and can evaluate the surrounding organs for related conditions.
MRCP (Magnetic Resonance Cholangiopancreatography)
This specialised MRI technique creates detailed images of the biliary and pancreatic ducts without using contrast agents. MRCP can detect small stones in the bile ducts that may be missed by ultrasound and can evaluate the entire biliary tree for abnormalities.
ERCP (Endoscopic Retrograde Cholangiopancreatography)
This procedure combines endoscopy and fluoroscopy to examine the bile ducts, pancreatic duct, and gallbladder. A flexible tube with a camera is passed through the mouth to the small intestine, and contrast dye is injected into the ducts. ERCP allows for both diagnosis and treatment, as stones can be removed during the procedure.
Treatment Options
Treatment approaches for gallstones depend on symptom severity, stone location, and patient-specific factors.
Non-Surgical Treatment
- Monitoring Asymptomatic Gallstones: For asymptomatic gallstones found incidentally, observation without treatment is the best approach. Regular follow-up appointments are recommended to monitor for any changes or the onset of symptoms that may require intervention only if indicated. Most patients can be discharged with advice.
- Dissolution Therapy: Oral medications such as ursodeoxycholic acid can dissolve certain cholesterol stones by altering bile composition. This approach has a high risk of recurrence and is not recommended as the standard of care. It is usually saved for patients in whom surgery is contraindicated and recurrences of gallbladder infection.
- Pain Management: For patients with infrequent, mild symptoms, pain medication and dietary modifications may provide relief. Anti-inflammatory drugs and antispasmodics can help control biliary colic during acute episodes. This approach does not remove stones but manages symptoms when surgery is contraindicated or deferred.
Surgical Treatment
- Laparoscopic Cholecystectomy: This minimally invasive procedure removes the gallbladder through small abdominal incisions. It represents the standard surgical treatment for symptomatic gallstones. Patients typically experience less post-operative pain, shorter hospital stays, and faster recovery compared to open surgery, usually returning to normal activities within 1-2 weeks.
- Open Cholecystectomy: Traditional surgical removal of the gallbladder through a larger abdominal incision may be necessary in certain situations. This approach is used when laparoscopic surgery is not feasible due to severe inflammation, scarring from previous surgeries, or anatomical variations. Recovery typically takes 4-6 weeks and involves a hospital stay of 3-5 days.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure removes stones from the bile ducts when they cause blockages. An endoscope is inserted through the mouth to the small intestine, where specialised tools can extract stones from the ducts. ERCP is typically performed for bile duct stones before or after cholecystectomy, depending on the clinical situation.
- Percutaneous Cholecystostomy: This procedure drains the gallbladder using a tube inserted through the skin. It is a temporary measure for patients unable to undergo immediate surgery, allowing inflammation to subside. The drainage tube remains in place until the patient’s condition improves enough for definitive treatment, usually within several weeks.
Are Your Symptoms Affecting Your Quality of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Prevention and Management
Lifestyle changes can help reduce the risk of gallstones and manage existing ones. Gradual weight loss prevents increased cholesterol secretion linked to rapid weight changes. Regular physical activity helps regulate metabolism and reduce gallstone risk. A diet high in fibre, fruits, vegetables, and whole grains, while low in saturated fats, promotes healthy bile composition. Eating regular meals stimulates normal gallbladder emptying, preventing stasis. For those with asymptomatic gallstones, avoiding fatty meals can reduce the risk of attacks. Staying well-hydrated supports proper bile flow.
Frequently Asked Questions
Can gallstones pass naturally?
Small gallstones may pass through the bile ducts into the intestine without causing symptoms. Stones smaller than 5mm occasionally move through the biliary system and exit the body in stool. However, larger stones typically cannot pass naturally and may require intervention if they cause blockages or symptoms.
Will I need to follow a special diet after gallbladder removal?
Most people do not require significant dietary changes after cholecystectomy. The liver continues to produce bile, which flows directly into the small intestine rather than being stored in the gallbladder. Some patients experience looser stools or digestive discomfort with fatty meals initially, but these symptoms typically improve within weeks to months as the body adapts.
Can pregnancy increase the risk of gallstones?
Pregnancy temporarily increases gallstone risk due to elevated oestrogen levels and decreased gallbladder emptying. Oestrogen raises cholesterol levels in bile, while progesterone reduces gallbladder contractions. These hormonal changes create conditions favourable for stone formation, particularly during the third trimester and immediately after delivery.
Is medication suitable for gallstone treatment?
Oral medications such as ursodeoxycholic acid can dissolve certain cholesterol stones by altering bile composition. This approach has a high risk of recurrence and is not recommended as the standard of care. It is usually saved for patients in whom surgery is contraindicated and recurrences of gallbladder infection.
Does removal of gallbladder affect absorption?
It actually doesn’t. Gallbladder is a reservoir and doesn’t produce the digestive juices needed for fat emulsification. Hence the digestion and absorption function is not affected after removal of gallbladder. It is actually a safe and effective strategy to prevent patients with gallstones from infection. Thus most patients with gallstones and have symptoms are advised for gallbladder removal.
Partnered Programmes & Insurance Plans
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.

















contact us
Please leave us a message and our friendly clinic staff will get back to you as soon as possible. For urgent or same day appointments, kindly call the clinic to arrange an appointment.
Our Clinic Locations
Ark Surgical Practice – Mount Elizabeth Medical Centre
3 Mount Elizabeth, #09-07
Singapore 228510
Monday to Friday: 9am – 5pm
Saturday: 9am – 12:30pm
Sunday & Public Holidays: Closed
Ark Surgical Practice – Mount Alvernia Hospital
820 Thomson Road,
Mount Alvernia Hospital, #06-52,
Medical Centre D, Singapore 574623
Wednesday: 9am – 12:30pm
Thursday: 2pm – 5pm





