- Abdominal bloatedness: This is the most common symptom for gallstones. Patients usually present with epigastric discomfort especially after a heavy meal and often misunderstood as indigestion. However, it is important to recognise that this symptom is also a symptom for gastric pain. Hence it is important to identify the trigger and the nature of such symptom to correlate with the underlying cause.
- Right upper quadrant pain: Pain typically occurs in the upper right portion of the abdomen and may radiate to the right shoulder or back. This pain often intensifies after eating fatty foods.
- Fever and chills: Body temperature may rise as the immune system responds to the inflammation. Chills frequently accompany the fever as the body attempts to raise its core temperature.
- Nausea and vomiting: The inflammatory process can trigger these symptoms due to the proximity of the gallbladder to the digestive tract. These symptoms often appear after meals.
- Abdominal tenderness: The area over the gallbladder becomes sensitive to touch or pressure. Patients may notice increased discomfort when pressed on the right upper abdomen.
- Jaundice: Yellowing of the skin and whites of the eyes occurs in some cases when the bile ducts become blocked. This happens when bile cannot flow normally through the biliary system.
Cholecystitis Treatment in Singapore
Cholecystitis is inflammation of the gallbladder, a small pear-shaped organ located beneath the liver that stores and concentrates bile. This condition occurs when bile becomes trapped in the gallbladder, leading to irritation and swelling of the gallbladder walls. Cholecystitis typically develops due to blockage of the cystic duct by gallstones, though it may also occur without stones present. The inflammation can cause significant abdominal pain and tenderness and, if left untreated, can lead to serious complications such as infection, gallbladder necrosis, or rupture of the gallbladder.


Symptoms of Cholecystitis
Patients with cholecystitis may experience a range of symptoms that vary in severity depending on the stage and extent of the inflammation.
Causes and Risk Factors
Cholecystitis develops due to various factors that can trigger inflammation in the gallbladder or obstruct bile flow.
Gallstones
These hardened deposits of digestive fluid form in the gallbladder and are the most common cause of cholecystitis. Gallstones can block the tube that carries bile from the gallbladder, causing bile to build up and leading to inflammation.
Bile duct problems
Narrowing or scarring of the bile ducts can impede bile flow and contribute to cholecystitis. These structural issues may result from previous surgeries or inflammatory conditions.
Tumours
Growths in the gallbladder or surrounding structures can obstruct bile flow and lead to cholecystitis. Both benign and malignant tumours may cause this obstruction.
Age
The risk of developing cholecystitis increases with age, particularly after 40. The gallbladder tends to function less efficiently with advancing years, making older adults more susceptible.
Gender
Women are more likely to develop gallstones and cholecystitis than men. Hormonal factors, including oestrogen, affect bile composition and gallbladder function.
Obesity
Excess weight increases cholesterol in the bile, raising the risk of gallstone formation. Obesity also alters gallbladder emptying patterns, contributing to bile stasis.
Pregnancy
Hormonal changes during pregnancy alter bile composition and slow gallbladder emptying. These changes increase the likelihood of gallstone formation and potential cholecystitis.
Diagnostic Methods
Physical examination
The doctor palpates the abdomen to check for tenderness, muscle rigidity, and a positive Murphy’s sign (pain when pressing on the gallbladder area while the patient takes a deep breath). This examination helps identify the location and potential cause of abdominal pain, guiding further diagnostic testing.
Ultrasound
This non-invasive imaging technique uses sound waves to create images of the gallbladder and surrounding structures. Ultrasound can detect gallstones, gallbladder wall thickening, pericholecystic fluid, and other signs of inflammation with high sensitivity and specificity, making it the first-line imaging test for suspected cholecystitis.
CT scan
Computed tomography creates detailed cross-sectional images of the abdomen, helping identify complications of cholecystitis such as perforation or abscess formation. CT scans can also detect other conditions that may mimic cholecystitis symptoms, providing differential diagnostic information when the diagnosis remains uncertain.
MRI/MRCP
Magnetic resonance imaging and magnetic resonance cholangiopancreatography provide detailed images of the biliary tract without radiation exposure. These techniques visualise bile ducts and can detect small gallstones, strictures, or tumours that may be missed by other imaging methods.
Treatment Options
Management of cholecystitis depends on the severity of symptoms, patient factors, and whether complications have developed.
Non-Surgical Treatment
- Fasting and intravenous fluids: Temporarily stopping oral intake allows the gallbladder to rest while IV fluids prevent dehydration. This approach helps reduce stimulation of gallbladder contraction and minimises pain during the acute phase of inflammation.
- Pain management: Analgesics help control abdominal pain and discomfort. Non-steroidal anti-inflammatory drugs or opioids may be used depending on pain severity and patient factors, with medication selection tailored to individual needs and contraindications.
- Antibiotics: If infection is present, antibiotics targeting common biliary tract pathogens are administered. These medications help control bacterial growth and prevent complications such as abscess formation or sepsis, particularly in moderate to severe cases.
- Gallstone dissolution medications: For patients who cannot undergo surgery, medications like ursodeoxycholic acid may help dissolve small cholesterol stones. This approach requires months to years of treatment and works only for certain types of stones.
Surgical Treatment
- Laparoscopic cholecystectomy: This minimally invasive procedure removes the gallbladder through small incisions in the abdomen. It represents the definitive treatment for cholecystitis in most cases, preventing recurrence by eliminating the source of inflammation.
- Open cholecystectomy: This traditional surgical approach involves removing the gallbladder through a larger abdominal incision. This method may be necessary for patients with severe inflammation, scarring from previous surgeries, or anatomical variations that make the laparoscopic approach challenging.
- Percutaneous cholecystostomy: A drainage tube placed through the skin into the gallbladder temporarily relieves pressure and drains infected bile. This procedure serves as a bridge to definitive surgery for critically ill patients who cannot immediately tolerate cholecystectomy or as palliation for those who are not surgical candidates.
- Endoscopic retrograde cholangiopancreatography (ERCP): This procedure allows removal of gallstones from the common bile duct using an endoscope. ERCP may be performed before cholecystectomy if stones have migrated from the gallbladder into the common bile duct, causing additional blockage.
Are Your Symptoms Affecting Your Quality of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Prevention and Management
Preventing cholecystitis involves reducing gallstone risk factors. Gradual weight loss helps maintain bile cholesterol balance, while a fibre-rich, low-fat diet supports gallbladder health. Regular physical activity aids weight management and gallbladder function. Those with gallstones can minimise attacks by avoiding high-fat foods and staying well-hydrated. Patients should discuss preventive cholecystectomy if symptoms arise. Patients who have had cholecystitis without gallbladder removal need regular monitoring to detect recurrence.
Frequently Asked Questions
What happens if cholecystitis is left untreated?
Untreated cholecystitis can progress to serious complications, including gallbladder perforation, abscess formation, or gangrene. These complications can lead to peritonitis, a life-threatening infection of the abdominal cavity. Chronic inflammation may also increase the risk of gallbladder cancer over time. Prompt medical attention reduces the risk of these adverse outcomes.
How will my digestion change after gallbladder removal?
Most people adapt well to life without a gallbladder. The liver continues to produce bile, which flows directly into the small intestine rather than being stored and concentrated in the gallbladder. Some patients experience digestive changes such as looser stools or more frequent bowel movements, particularly after fatty meals. These symptoms typically improve within a few months as the body adjusts to the new digestive pattern.
Can cholecystitis recur after antibiotic treatment?
Cholecystitis can recur after antibiotic treatment if the gallbladder is not removed. While antibiotics help clear the infection, they do not eliminate the underlying issue—most often gallstones blocking bile flow. Without surgical removal, inflammation may return, especially if gallstones continue to obstruct the gallbladder.
Partnered Programmes & Insurance Plans
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.

















contact us
Please leave us a message and our friendly clinic staff will get back to you as soon as possible. For urgent or same day appointments, kindly call the clinic to arrange an appointment.
Our Clinic Locations
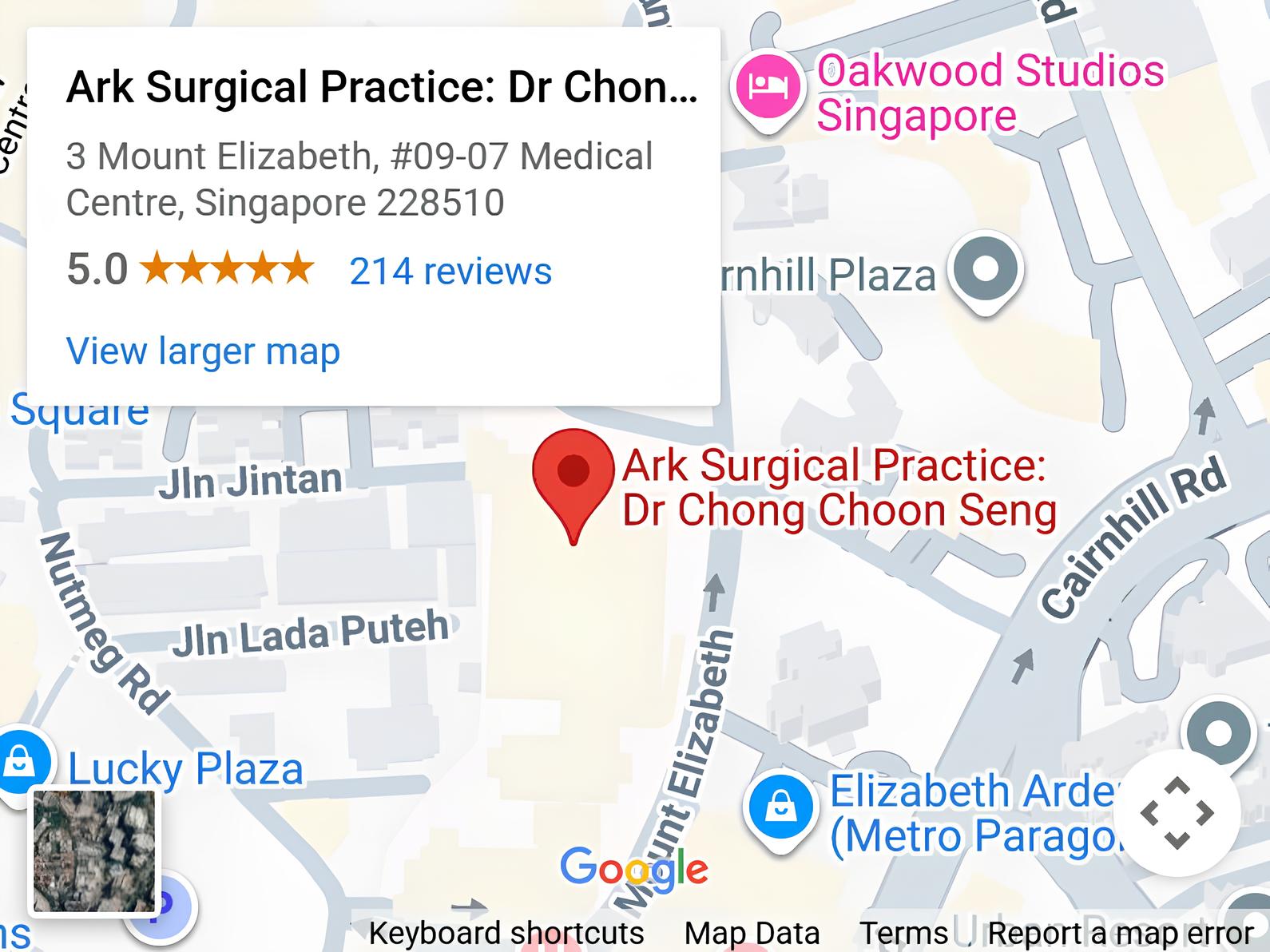
Ark Surgical Practice – Mount Elizabeth Medical Centre
3 Mount Elizabeth, #09-07
Singapore 228510
Monday to Friday: 9am – 5pm
Saturday: 9am – 12:30pm
Sunday & Public Holidays: Closed
Ark Surgical Practice – Mount Alvernia Hospital
820 Thomson Road,
Mount Alvernia Hospital, #06-52,
Medical Centre D, Singapore 574623
Wednesday: 9am – 12:30pm
Thursday: 2pm – 5pm