Do you feel tissue protruding from your anal opening during bowel movements? Rectal prolapse involves the rectum’s full thickness sliding through the anal opening, while hemorrhoids are swollen blood vessels within or around the anus. Both conditions cause tissue protrusion from the anal canal, leading many patients to mistake one for the other. The distinction matters because rectal prolapse requires surgical intervention in most cases, whereas hemorrhoids often respond to conservative treatment.
Colorectal surgeons use examination techniques to differentiate these conditions. During rectal prolapse, concentric circular folds of tissue appear when straining, contrasting with the radial folds and purple-tinged appearance of prolapsed hemorrhoids.
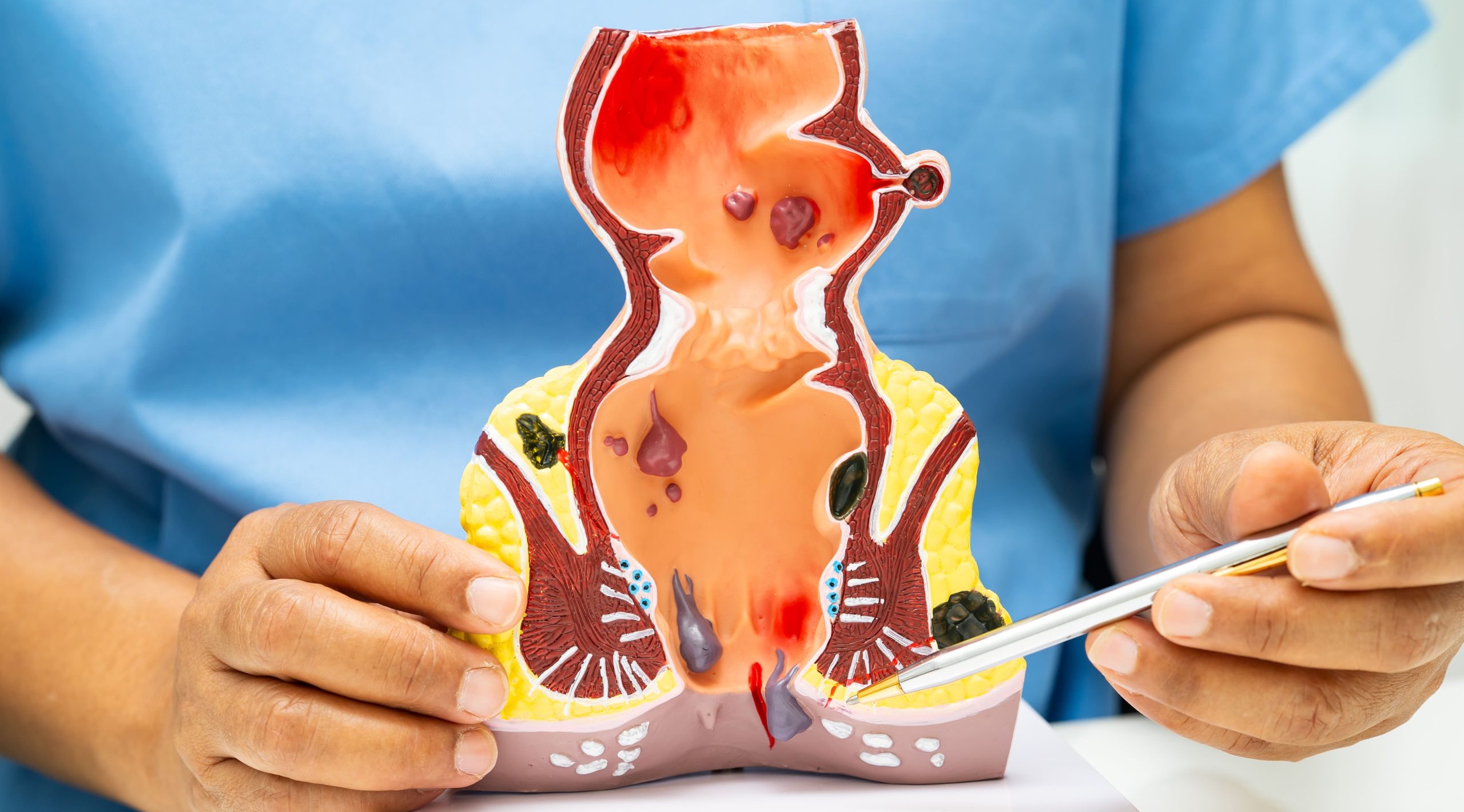
Anatomical Differences
Hemorrhoids develop from cushions of blood vessels naturally present in the anal canal. Internal hemorrhoids originate above the dentate line, where no pain receptors exist. External hemorrhoids form below this line in tissue containing numerous nerve endings, explaining why thrombosed external hemorrhoids cause severe pain.
Rectal prolapse occurs when the rectum loses its normal attachments inside the pelvis. The rectal wall telescopes through the anus, bringing all layers of the rectal wall with it. This differs fundamentally from hemorrhoids, which involve only the blood vessels and surrounding tissue, not the entire rectal wall structure.
Three types of rectal prolapse exist based on the extent of tissue displacement:
- Internal prolapse (intussusception) remains inside the rectum without emerging through the anus
- Mucosal prolapse involves only the rectal lining protruding through the anal opening
- Full-thickness prolapse brings the entire rectal wall through the anus
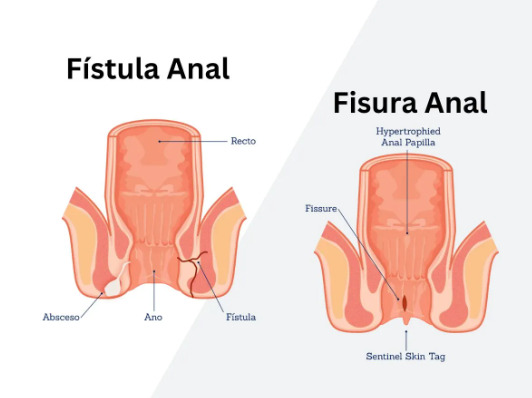
Visual and Physical Characteristics
Prolapsed hemorrhoids appear as distinct lumps or grape-like clusters protruding from the anus. The tissue typically shows a purple or dark red color when thrombosed, or pink when not inflamed. Individual hemorrhoids maintain separation from each other, and gentle examination reveals their origin from specific points within the anal canal.
Rectal prolapse presents as a uniform, cylindrical mass of tissue extending from the anus. The prolapsed segment displays concentric rings or circular folds running around its circumference. The tissue appears pink or red, similar to the intestinal lining, and forms a continuous tube rather than separate lumps. Manual examination reveals the prolapse involves the entire circumference of the anal opening.
Size provides another distinguishing feature. Hemorrhoids typically extend a few centimeters from the anal verge, even when severely prolapsed. Rectal prolapse can produce significantly more protruding tissue, particularly in complete prolapse cases. The prolapsed rectum often requires manual reduction after bowel movements, while many hemorrhoids retract spontaneously.
Symptoms Comparison
Hemorrhoid symptoms vary based on location and severity. Internal hemorrhoids cause painless bleeding, typically bright red blood on toilet paper or dripping into the toilet bowl. Grade 3 and 4 internal hemorrhoids prolapse during defecation, requiring manual reduction in advanced cases. External hemorrhoids produce pain, swelling, and difficulty with hygiene when thrombosed.
Rectal prolapse generates distinct symptoms beyond simple tissue protrusion. Patients experience a sensation of incomplete evacuation even after bowel movements. Mucus discharge soils undergarments continuously, requiring frequent pad changes. Fecal incontinence affects patients, ranging from gas leakage to complete loss of solid stool control.
The progression timeline differs between conditions. Hemorrhoids often develop acutely during pregnancy, heavy lifting, or constipation episodes, with symptoms fluctuating based on bowel habits and diet. Rectal prolapse typically progresses gradually over months or years, beginning with internal intussusception before advancing to external prolapse.
💡 Did You Know?
The rectum contains specialized sensory receptors that distinguish between gas, liquid, and solid stool – a function often impaired in rectal prolapse but preserved in hemorrhoids.
Causes and Risk Factors
Hemorrhoids develop from increased pressure in the anal cushions. Chronic constipation forces repeated straining during defecation, engorging the hemorrhoidal vessels. Pregnancy increases pelvic pressure and hormonal changes that weaken supporting tissues. Prolonged sitting, particularly on the toilet, allows blood to pool in the anal cushions. Heavy lifting and chronic cough create repeated intra-abdominal pressure spikes.
Rectal prolapse results from weakness in the pelvic floor muscles and ligaments supporting the rectum. Childbirth, especially multiple vaginal deliveries, stretches and damages the pelvic floor structures. Chronic straining from constipation gradually weakens the rectal attachments. Neurological conditions affecting the pelvic nerves, including spinal cord injuries and multiple sclerosis, predispose to prolapse development.
Age-related tissue changes affect both conditions differently. Hemorrhoids can occur at any age but peak during pregnancy and middle age. Rectal prolapse shows two distinct age peaks: young children and older adults, with women affected more frequently than men in the adult population. Connective tissue disorders like Ehlers-Danlos syndrome specifically increase rectal prolapse risk without necessarily affecting hemorrhoid development.
Diagnostic Approaches
Physical examination in the knee-chest or left lateral position allows direct visualization of both conditions. Colorectal surgeons ask patients to strain or bear down during examination, recreating the prolapse for assessment. Digital rectal examination evaluates sphincter tone, which remains normal in hemorrhoids but often weakens with rectal prolapse.
Anoscopy provides visualization of the anal canal and lower rectum. The procedure takes 2-3 minutes in clinic without sedation, revealing internal hemorrhoids’ location, size, and degree of prolapse. The anoscope also identifies other anal pathology including fissures, fistulas, or masses that might complicate treatment planning.
Defecography or dynamic MRI captures the defecation process in real-time, particularly valuable for internal rectal prolapse diagnosis. These imaging studies reveal rectocele, enterocele, or sigmoid prolapse occurring simultaneously with rectal prolapse. The studies measure the anorectal angle and pelvic floor descent during straining, quantifying the degree of pelvic floor dysfunction.
⚠️ Important Note
Colonoscopy may be recommended for patients over 50 or those with rectal bleeding to exclude colorectal cancer before attributing symptoms solely to hemorrhoids or prolapse. A healthcare professional can determine the appropriate diagnostic approach.
Treatment Options
Conservative Management
Hemorrhoids respond to dietary fiber supplementation of 25-35 grams daily, increasing stool bulk and reducing straining. Sitz baths in warm water for 10-15 minutes three times daily reduce hemorrhoidal congestion and spasm. Topical preparations containing local anesthetics provide temporary symptom relief, though corticosteroid creams should limit use to 7-10 days to prevent anal skin atrophy.
Rectal prolapse rarely improves with conservative measures alone, though pelvic floor physiotherapy strengthens supporting muscles in mild cases. Biofeedback training teaches proper defecation techniques, reducing straining that worsens prolapse. Stool softeners prevent constipation-related straining, potentially slowing prolapse progression in early stages.
Procedural Interventions
Rubber band ligation treats Grade 1-3 internal hemorrhoids by placing elastic bands above the dentate line, causing hemorrhoid necrosis within 5-7 days. The procedure requires no anesthesia and achieves success in many patients, though 2-3 sessions spaced 2 weeks apart may be necessary for multiple hemorrhoids.
Sclerotherapy injects phenol or polidocanol directly into internal hemorrhoids, causing fibrosis and fixation to underlying tissue. The technique works well for Grade 1-2 hemorrhoids with bleeding as the primary symptom. Infrared coagulation applies focused heat to hemorrhoid tissue, creating controlled necrosis similar to banding but suitable for smaller hemorrhoids.
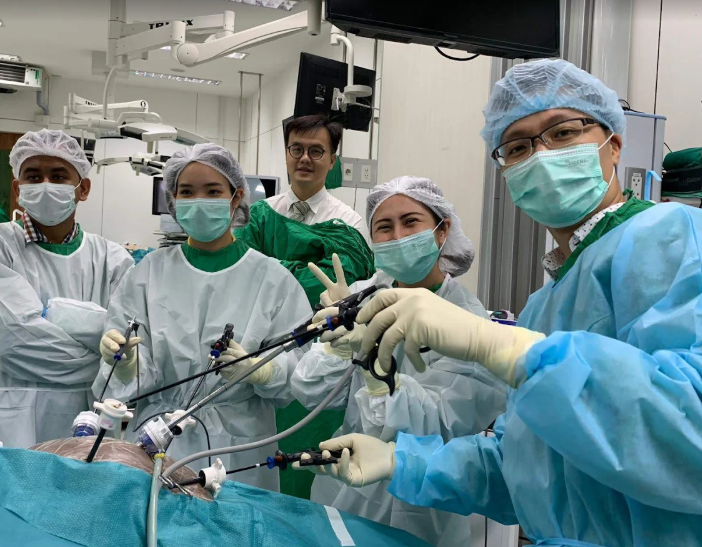
Surgical Solutions
Hemorrhoidectomy removes prolapsing internal and external hemorrhoids completely, providing treatment for Grade 3-4 hemorrhoids. Surgeons use either conventional excision, harmonic scalpel, or LigaSure devices to remove hemorrhoid tissue while preserving adequate anal cushion for continence. Recovery requires 2-4 weeks, with pain management important during the first week post-operatively.
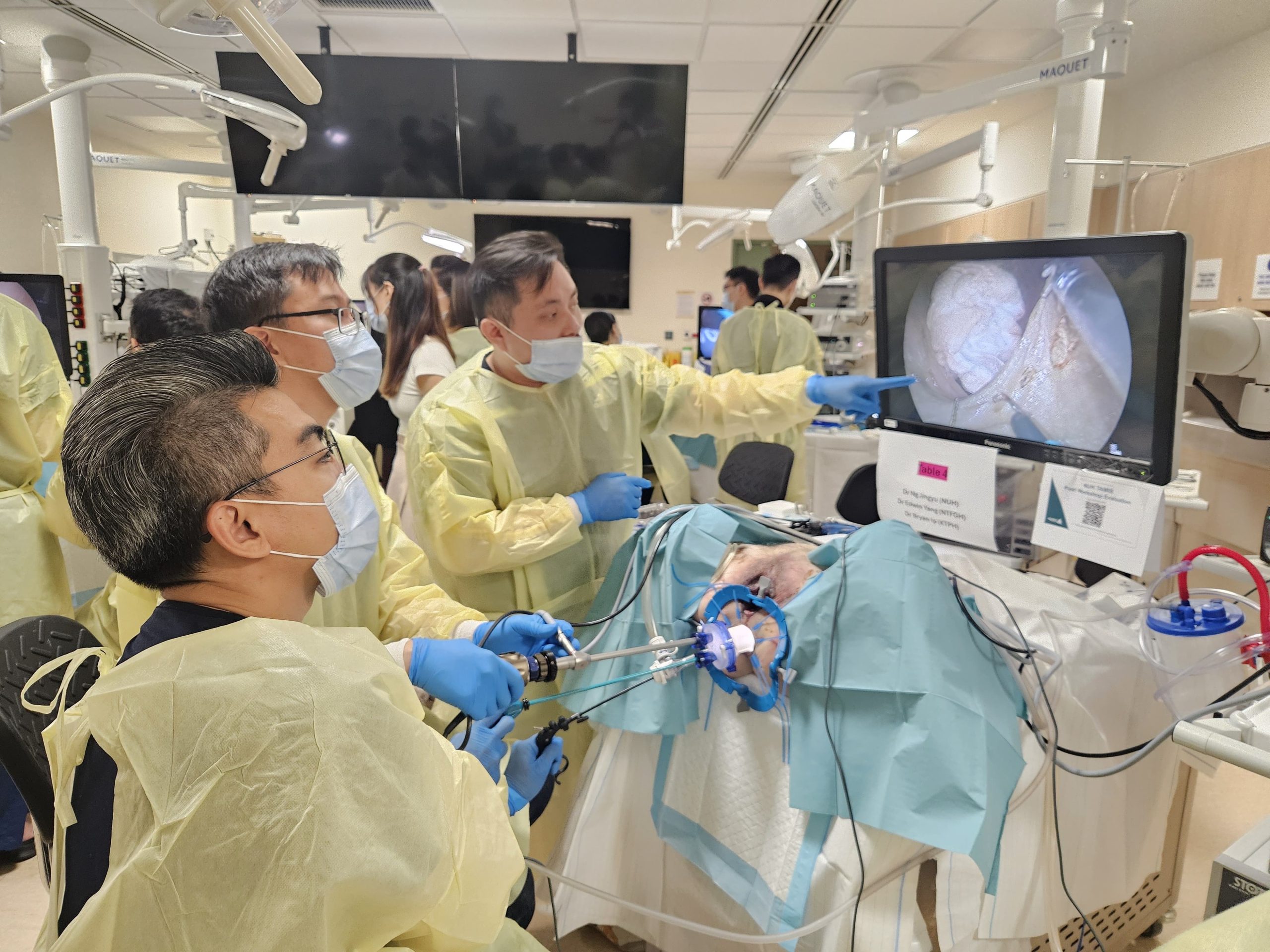
Rectal prolapse surgery approaches the problem through abdominal or perineal routes. Abdominal rectopexy, performed laparoscopically in most cases, secures the rectum to the sacrum using sutures or mesh. This approach suits younger patients with good surgical risk profiles, achieving low recurrence rates. The surgery preserves normal bowel length while correcting the anatomical defect.
Perineal procedures including Altemeier’s procedure (perineal rectosigmoidectomy) remove the prolapsing segment through the anus without abdominal incisions. These approaches suit elderly patients or those with significant medical comorbidities preventing abdominal surgery. Delorme’s procedure strips the rectal mucosa and plicates the muscle wall, appropriate for shorter prolapse segments under 8 centimeters.
Complications if Untreated
Untreated hemorrhoids lead to chronic blood loss causing iron deficiency anemia. Thrombosed hemorrhoids develop acute clots within the hemorrhoidal vessels, producing severe pain before gradually resolving. Strangulated hemorrhoids occur when prolapsed tissue becomes trapped outside the anus, cutting off blood supply and potentially causing tissue death.
Rectal prolapse progressively worsens without treatment, advancing from occasional prolapse during defecation to constant protrusion requiring frequent manual reduction. The exposed rectal mucosa develops ulceration and bleeding from chronic trauma. Incarceration occurs when the prolapsed segment cannot be reduced, causing bowel obstruction requiring emergency surgery.
Long-term prolapse stretches the anal sphincters, producing irreversible damage even after surgical repair. Fecal incontinence can persist in some patients post-operatively, particularly those with prolonged prolapse duration before treatment. The psychological impact includes social isolation and reduced quality of life from unpredictable bowel control loss.
✅ Quick Tip
Keep a symptom diary documenting prolapse episodes, bleeding patterns, and bowel habits before your specialist consultation to aid accurate diagnosis.
What Our Colorectal Surgeon Says
Patients often delay seeking treatment due to embarrassment, allowing both conditions to progress unnecessarily. Current treatment options provide good outcomes with minimal discomfort when addressed early. Accurate diagnosis is important – specific examination findings help distinguish hemorrhoids from prolapse.
Surgical timing matters significantly for rectal prolapse outcomes. Operating before chronic sphincter damage occurs preserves continence function post-operatively. For hemorrhoids, procedures are typically recommended only after failed conservative management or when prolapse significantly impacts daily activities.
Current techniques including THD (transanal hemorrhoidal deartialization) and laparoscopic ventral rectopexy minimize post-operative pain while providing durable results. Recovery protocols emphasizing early mobilization and multimodal analgesia have improved the post-operative experience compared to traditional approaches.
Putting This Into Practice
- Document your symptoms in detail, noting whether tissue protrudes during bowel movements only or remains external constantly, helping your doctor differentiate between conditions
- Photograph any protruding tissue (if comfortable) to show your colorectal surgeon, as symptoms may not be present during examination
- Consider modifying toilet habits by limiting sitting time and avoiding phone use that prolongs toilet sessions
- Consider increasing dietary fiber gradually through whole grains, vegetables, and fiber supplements while maintaining adequate water intake
- Discuss pelvic floor exercises with your healthcare provider, who can guide you on appropriate techniques and frequency
When to Seek Professional Help
- Tissue protrusion from the anus that requires manual pushing back inside
- Rectal bleeding persisting beyond one week or recurring frequently
- Inability to distinguish between gas, liquid, and solid stool
- Mucus discharge requiring pad use or causing skin irritation
- Pain during bowel movements lasting more than several days
- Sensation of incomplete evacuation despite successful defecation
- Any sudden change in bowel habits lasting more than two weeks
- Visible tissue remaining outside the anus between bowel movements
Commonly Asked Questions
Can hemorrhoids turn into rectal prolapse over time?
Hemorrhoids and rectal prolapse remain distinct conditions with different underlying causes. Hemorrhoids involve blood vessel enlargement while prolapse results from pelvic floor weakness. Untreated hemorrhoids don’t transform into prolapse, though both conditions can coexist in the same patient.
Why does my doctor need to examine me during straining?
Straining recreates the prolapse or hemorrhoid protrusion that occurs during defecation. Many cases appear normal at rest but reveal pathology only during bearing down. This dynamic examination provides important diagnostic information that static examination misses.
Which condition has better treatment outcomes?
Both conditions can achieve good results with appropriate treatment. Hemorrhoid procedures like banding may be successful in many patients with minimal recovery time. Rectal prolapse surgery, while more involved, can provide durable repair with low recurrence rates using current techniques.
Can these conditions resolve without treatment?
Small internal hemorrhoids may improve with dietary changes and proper bowel habits. Rectal prolapse typically does not resolve spontaneously and may progressively worsen without intervention. Treatment of both conditions can help prevent complications and may provide better long-term outcomes.
How long before I can return to normal activities after surgery?
Hemorrhoid procedures may allow return to desk work within 3-5 days and full activities by 2 weeks. Laparoscopic rectal prolapse surgery may require 1-2 weeks before returning to light activities and 4-6 weeks for complete recovery including heavy lifting. Recovery times can vary and should be discussed with your healthcare provider.
Conclusion
Proper diagnosis differentiates rectal prolapse from hemorrhoids through clinical examination. Surgery provides definitive treatment for rectal prolapse, while hemorrhoids often respond to conservative management. Early evaluation helps preserve bowel function and prevent complications.
If you’re experiencing tissue protrusion requiring manual reduction or have persistent rectal bleeding, a MOH-accredited colorectal surgeon can provide accurate diagnosis and treatment options.